All published articles of this journal are available on ScienceDirect.
Factors Influencing Adolescent Resilience and Human Immunodeficiency Virus-Acquired Immune Deficiency Syndrome Prevention Behavior: A Cross-sectional Study of Adolescents in DKI Jakarta Province, Indonesia
Abstract
Background
The incidence of human immunodeficiency virus (HIV)-acquired immune deficiency syndrome (AIDS) remains high in Indonesia. Therefore, HIV-AIDS prevention and control programs have been established for adolescents aged 15–24 years based on the United Nations Sustainable Development Goals. Internal risk factors related to risky sexual behavior and external risk factors associated with exposure to pornography through the media are major hurdles that need to be overcome in efforts to prevent HIV-AIDS among adolescents. Meanwhile, individual protective factors through self-control and adolescent resilience strongly impact the enhancement of HIV-AIDS prevention behavior. This study aimed to determine whether internal and external risk factors and individual and sociocultural protective factors exert influences on adolescent resilience and HIV-AIDS prevention behavior among adolescents.
Methods
This research employed a descriptive quantitative design with a cross-sectional approach. The population consisted of high school students aged 15–19 years in Jakarta, and a sample of 619 students was taken through proportional stratified random sampling. Inferential analysis was conducted using partial least squares structural equation modeling.
Results
The data analysis revealed that adolescent resilience (β-value = 0.423; t = 12.129), internal risk factors (β-value = 0.292; t = 10.903), and external risk factors (β-value = -0.088; t = 6.127) most significantly influenced HIV-AIDS prevention behavior, with significant negative impacts. The sub-variable that most strongly determined the presence of HIV-AIDS prevention behavior (Y2) was self-control (λ = 0.983), and the one that did so most weakly was negative cognition (λ = 0.875).
Conclusion
Adolescent resilience is a crucial factor in enhancing HIV-AIDS prevention behavior among adolescents as it influences adolescents’ beliefs, boosts their self-confidence, fosters emotional insight, and develops social skills and empathy toward others. Thus, enhancing it through HIV-AIDS prevention programs is essential.
1. INTRODUCTION
The cases of human immunodeficiency virus (HIV)-acquired immune deficiency syndrome (AIDS) continue to pose a global challenge despite prevention and control efforts in response to the epidemic. AIDS is an immune system disorder and infectious disease caused by HIV. By the end of 2020, there was an estimated 38 million people living with HIV (PLHIV) worldwide, and there are approximately 1.5 million new HIV infections occurring each year, according to the United Nations Programme on HIV/AIDS [1, 2]. Indonesia, one of the Asian countries with the highest number of PLHIV, contributed 427,201 HIV infections and 131,417 AIDS cases to the total number of cases [3]. The highest number of HIV cases (9,675) was reported in the DKI Jakarta region [4]. The adolescent age group (10–19 years) contributes approximately 7% to the total number of PLHIV [5].
The high incidence of HIV-AIDS in Indonesia has led to the establishment of prevention and control programs targeting adolescents aged 15–24 in the country, based on the Sustainable Development Goals. This phenomenon is driven by the challenges posed to adolescents by changes in information technology (IT), such as the emergence of dating applications such as Blumber and Tinder. These social apps are designed to facilitate meetings between unfamiliar individuals looking for partners or friends, altering perceptions and leading to influences from the environment, thus encouraging risky behavior [6]. Many adolescents using such applications may face increased sexual health risks [7-9]. Various sources attribute the high incidence of HIV-AIDS to risky sexual behavior, defined as sexual activity that can make someone risky to sexually transmitted infections (STIs), including HIV, and unplanned pregnancy [10].
The present study highlighted HIV-AIDS prevention behavior, particularly in the context of preventing risky sexual behavior. In Indonesia, HIV-AIDS prevention behavior involves both passive responses (knowledge, attitudes, and perceptions) and active responses (actions taken to prevent HIV infection), including abstaining from premarital sex, being faithful to one partner, and avoiding intravenous drug use [11]. Adolescents with limited adaptive abilities are likelier to engage in risky behavior (including risky sexual behavior) than in HIV-AIDS prevention behavior [12, 13].
Risk factors are divided into internal and external factors [14]. Adolescent-related internal risk factors for HIV-AIDS risk behavior include age, gender, education, ethnicity, puberty index, daily allowance, dating history, and risky sexual behavior [15, 16]. On the other hand, adolescent-related external risk factors for HIV-AIDS risk behavior can be divided into interpersonal and situational factors. The interpersonal factors include inadequate parental support in addressing adolescent issues, the failure of parents and families to provide the main support structure for adolescent growth, transitioning into adulthood with a large family structure, low parental education, occupationally busy parents, and low family income. These factors also contribute to risky sexual behavior, early pregnancies, the risk of sexually transmitted infections other than HIV, and drug abuse [17]. Parental roles in educating children are strongly influenced by their educational levels [18], which may also affect parental control in relation to adolescent premarital sexual behavior [19].
Situational external risk factors arise from access to IT and exposure to pornography through the media [15]. Changes in IT alter adolescents’ perceptions and behavior, leading these to unhealthy directions [20]. Some studies suggest that the higher the level of pornography addiction, the greater risky sexual behavior may be in adolescents [21].
In addition to risk factors, identifying protective factors is essential for analyzing appropriate HIV-AIDS prevention behavior. Protective factors for HIV-AIDS prevention behavior in adolescents are divided into individual and sociocultural factors. Individual protective factors influencing HIV-AIDS prevention behavior in adolescents include knowledge, attitudes, subjective norms, self-control, self-esteem, and self-efficacy [15]. Adolescent challenges in developing the first four of these factors, as well as HIV-AIDS prevention behavior, are influenced by the transitional period adolescents are in, which is a critical stage due to the rapid physical, mental, and intellectual changes that they experience [22]. Adolescents with perceived low self-esteem are likelier to engage in negative behavior, such as premarital sexual relationships than those with perceived high self-esteem.
Sociocultural protective factors pertaining to family and community also play a crucial role. Families can be a protective factor against behavior that may promote HIV infection because a well-functioning family can shape healthy behavior in the children, protecting them from risky sexual behavior that may increase their risk of HIV infection [15]. The school community, as a second environment after the family, can also be a protective factor involving the roles of teachers and school nurses in promoting prevention efforts and active participation by adolescents in HIV-AIDS prevention programs at school [23].
Various national and international HIV-AIDS prevention programs have been launched to save future generations from the scourge of infectious diseases. The ultimate goal of these programs is to build adolescent resilience, which is the ability to adapt to various risks and stressful situations to avoid negative health or social impacts and to grow successfully [24, 25]. Resilient adolescents can function competently and demonstrate effective HIV-AIDS prevention behavior when exposed to significant risks [26]. Adolescent resilience is crucial for promoting and maintaining adolescents’ well-being, especially their psychological well-being, enabling them to employ defense mechanisms in the face of threats or challenges that may arise throughout their lives [27]. The present study explored it in relation to strength-based concepts for adaptation, trends, digital lifestyles, and their connections to shaping HIV-AIDS prevention behavior. Risk factors, protective factors, adolescent resilience, and HIV-AIDS prevention behavior place adolescents at the center of the HIV-AIDS epidemic within the family, peer networks, broader networks, and society [28]. Based on this problem background, the researchers examined and explored the factors influencing adolescent resilience and HIV-AIDS prevention behavior in DKI Jakarta Province, Indonesia.
2. METHODS
The present study adopted a descriptive quantitative design with a cross-sectional approach using structural equation modeling to investigate the factors influencing adolescent resilience and HIV-AIDS prevention behavior [29, 30]. Adolescent resilience is influenced by internal factors, external factors, sociocultural protective factors, and individual protective factors.
The study population consisted of 386,670 adolescents currently attending high school (senior high school or vocational school) in DKI Jakarta Province [31]. Sample size calculations using G*Power based on Kang [32] and the minimum sample from Hair et al. [33] resulted in a sample of 619 students. Proportional stratified random sampling was used for respondent selection. Twenty schools (10 senior high schools and 10 vocational schools) located in five administrative cities (South Jakarta, Central Jakarta, North Jakarta, West Jakarta, and East Jakarta) within the working area of the Jakarta Provincial Education Office were randomly selected. From these schools, respondents were chosen based on the following inclusion criteria: adolescents aged 15–19, living with their parents in DKI Jakarta, without physical disabilities and mental disorders, able to communicate in Bahasa Indonesia, are in a romantic relationship or have experienced being in one, have undergone puberty (boys have experienced wet dreams; girls have menstruated), and have never been married. Participation in the study was entirely voluntary. Informed consent was obtained from all respondents, and they were clearly informed that they could refuse to participate or withdraw from the study at any time without any consequences. This ensured that the students’ participation was based on their own free will.
The primary inconvenience for respondents was the time spent completing the questionnaire. To mitigate this, we scheduled data collection sessions in coordination with the respondents' daily activities, ensuring minimal disruption. We also provided breaks to prevent fatigue and stress, allowing respondents to eat, drink, or use the restroom as needed. Additionally, we ensured the ethical handling of data and did not exploit respondent information for any external gains.
The data collection instrument was a questionnaire adopted from previous researchers covering the following: (1) respondent demographic data; (2) risky sexual behavior (33 statement items) [34]; (3) exposure to media pornography (23 statement items) [34]; (4) coping strategies (33 statement items) [35]; (5) attitudes toward HIV-AIDS prevention (15 statement items) [36]; (6) self-control (13 statement items) [37]; (7) knowledge about HIV-AIDS (18 statement items) [38]; (8) self-esteem (10 statement items) [39]; (9) self-efficacy (21 statement items) [40]; (10) family resilience (32 statement items) [41]; (11) adolescent resilience (49 statement items) [42]; and (12) HIV-AIDS prevention behavior (18 statement items) [22]. The validity and reliability of the questionnaire were tested on 30 adolescents who met the criteria.
A rigorous translation process was undertaken to ensure the accuracy and cultural relevance of the instruments. The translation involved the forward translation of the questionnaires from English to Bahasa Indonesia by bilingual experts, followed by a backward translation to English by a different set of bilingual experts. Discrepancies between the original and back-translated versions were reconciled through discussions among the translators and the research team. The translated questionnaires were then reviewed by a panel of experts for cultural and contextual appropriateness. Pre-testing of the translated questionnaires was conducted on a Senior High School group of adolescents who met the inclusion criteria, and adjustments were made based on their feedback to ensure clarity and relevance.
Given the involvement of minors in this study, obtaining informed consent was a critical aspect of our methodology. Consent forms were provided to the parents or guardians of the potential respondents, detailing the study’s objectives, procedures, and the sensitive nature of some of the topics (such as sexual health and HIV/AIDS prevention). Only students whose parents or guardians provided written consent were allowed to participate. Additionally, we sought and obtained assent from students themselves, ensuring that they understood the study and voluntarily agreed to participate.
The pre-testing phase revealed that most respondents, including younger students, could complete the question- naire within 45-60 minutes without showing signs of fatigue or disengagement. Feedback from pre-testing indicated that the questions were comprehensible to the younger respondents. During the actual data collection, members of the research team were present to offer any necessary clarifications, ensuring that all students were able to read and understand the questions effectively.
Validity (X1.8, X2.8, X3.1, X3.2, X3.3, X3.4, X3.5, X3.6, X4.1, Y1, and Y2) was confirmed, with the validity coefficient results ranging from 0.407 to 0.843, 0.369 to 0.873, 0.457 to 0.817, 0.494 to 0.807, 0.550 to 0.784, 0.411 to 0.757, 0.473 to 0.874, 0.467 to 0.816, 0.404 to 0.855, 0.396 to 0.946, and 0.535 to 0.943, respectively, all greater than the tabulated r value of 0.367. The reliability values, based on Cronbach’s alpha values, were 0.933, 0.924, 0.960, 0.925, 0.899, 0.900, 0.870, 0.929, 0.966, 0.979, and 0.966, respectively.
The data were collected from the first week of April 2023 to the beginning of October 2023. The research team visited the selected schools during regular school hours, coordinating with school administrators to minimize disruption to the students’ academic schedules. Question- naires were distributed to eligible students in classroom settings during designated time slots agreed upon with school authorities, typically during study hall periods or immediately after school hours. Students were given approximately 45-60 minutes to complete the question- naire in a supervised environment to ensure privacy and address any questions. The research team was present during the administration to provide clarification if needed and to collect the completed questionnaires, ensuring a high response rate and allowing for immediate verification of questionnaire completeness. The data collection process took approximately six months.
The data analysis involved descriptive analysis to assess the categorical data (frequency distribution and percentage) and numerical data (mean or median, range, and standard deviation) of the respondent characteristics, risk factors, protective factors, adolescent resilience, and HIV-AIDS prevention behavior. The researchers conducted inferential analyses using partial least squares structural equation modeling algorithms with SmartPLS 3.0 software [43, 44]. The goal was to identify the variables that influence adolescent resilience and HIV-AIDS prevention behavior the most. The research framework for the first stage is illustrated in Fig. (1).
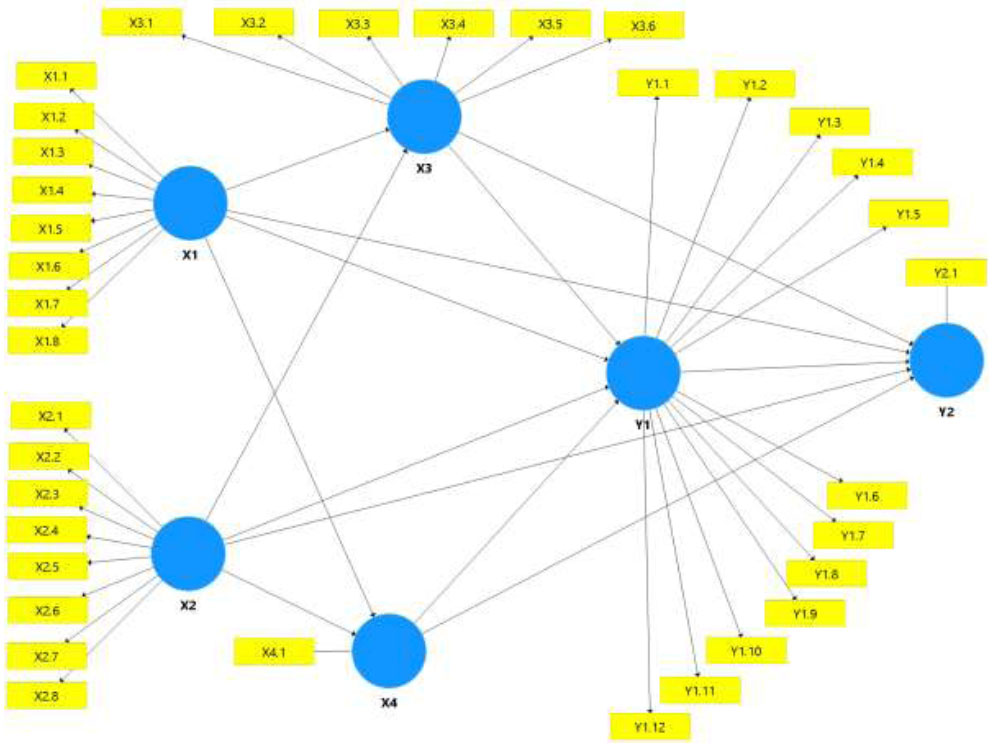
Research conceptual framework.
Note:
X1: Internal risk factors: X2.5: Father’s occupation: Y1.1: Self-confidence.
X1.1: Age: X2.6: Family income: Y1.2: Emotional insight/awareness.
X1.2: Gender: X2.7: Socioeconomic conditions of the environment: Y1.3: Negative cognition.
X1.3: Ethnicity: X2.8: Exposure to pornography from the media: Y1.4: Social skills.
X1.4: Allowance: X3: Individual protective factors: Y1.5: Empathy.
X1.5: Living with family: X3.1: Coping strategies: Y1.6: Family attachment.
X1.6: Dating history: X3.2: Attitudes toward HIV-AIDS prevention: Y1.7: Family presence/existence.
X1.7: Duration of dating: X3.3: Self-control: Y1.8: Friend attachment.
X1.8: Risky sexual behavior: X3.4: Knowledge about HIV-AIDS: Y1.9: Friend presence/existence.
X2: External risk factors: X3.5: Self-esteem: Y1.10: School environment.
X2.1: Family type: X3.6: Self-efficacy: Y1.11: School attachment.
X2.2: Mother’s education: X4: Sociocultural protective factor: Y1.12: Community attachment.
X2.3: Father’s education: X4.1: Family resilience: Y2: HIV-AIDS prevention behavior.
X2.4: Mother’s occupation: Y1: Adolescent resilience: Y2.1: HIV-AIDS prevention behavior.
3. RESULTS
3.1. Adolescent Demographic Characteristics (Internal Factors) and Interpersonal External Factors
Table 1 shows that most of the respondents were 16 years old (n = 317; 51.2%), female (n = 371; 59.9%), of Javanese ethnicity (n = 243; 39.3%), and had a low daily allowance of < Rp.25,197.00 (n = 334; 54%). About 90.5% (n = 600) lived with their parents, and 66.1% (n = 409) had a history of dating, with 54.4% having had a long duration of dating. Finally, 59.3% exhibited low-risk sexual behavior. Based on these data, it was evident that the adolescents had diverse characteristics influenced by their internal environments. The significance of the results indicates that adolescents in DKI Jakarta generally engage in dating behavior with intensive and prolonged frequency, even though less than half of them are likely to exhibit high-risk sexual behavior.
Most of the respondents had fathers with Senior High School education levels (61.6%) and non-governmental occupations such as laborers, entrepreneurs, and private employees (n = 593; 95.8%). Most mothers also had Senior High School education levels (57.2%) and non-governmental occupations (n = 597; 96.4%). Nuclear family types were predominant (n = 560; 90.5%). About 62% of the respondents had a family income below the regional minimum wage, and 47.8% had good socio- economic conditions and environments. Finally, 59.9% of the respondents reported low exposure to pornography from the media. These results may be due to low parental monitoring as nearly 100% of the parents had a Senior High School education and were employed. Thus, they suggest that external risk factors such as exposure to pornography require attention.
| Internal Risk Factor | - | Frequency | % |
|---|---|---|---|
| Age (years old) | 15 | 48 | 7.8 |
| - | 16 | 317 | 51.2 |
| - | 17 | 197 | 31.8 |
| - | 18 | 50 | 8.1 |
| - | 19 | 7 | 1.1 |
| Sex | Male | 248 | 40.1 |
| - | Female | 371 | 59.9 |
| Ethnicity | Others | 87 | 14.1 |
| - | Betawi | 196 | 31.7 |
| - | Sundanese | 93 | 15.0 |
| - | Javanese | 243 | 39.3 |
| Daily allowance | Low (< Rp.25,197.00) | 334 | 54.0 |
| - | High (≥ Rp.25,197.00) | 285 | 46.0 |
| Living with family | Other family | 19 | 9.5 |
| - | Parents | 600 | 90.5 |
| Dating history | Have | 210 | 33.9 |
| - | Used to have (broke up) | 409 | 66.1 |
| Duration of dating | Short < 6 months | 282 | 45.6 |
| - | Long ≥ 6 months | 337 | 54.4 |
| Risky sexual behavior | High-risk sexual behavior ≥ 48.37 | 252 | 40.7 |
| - | Low-risk sexual behavior < 48.37 | 367 | 59.3 |
| External Risk Factor | - | Frequency | % |
| Exposure to pornography from media | High exposure to pornography ≥ 35.24 | 248 | 40.1 |
| - | Low exposure to pornography < 35.24 | 371 | 59.9 |
| Father’s education | Elementary school | 55 | 8.9 |
| - | Junior high school | 67 | 10.8 |
| - | Senior high school | 381 | 61.6 |
| - | Higher education | 116 | 18.7 |
| Father’s occupation | Non-civil servant | 593 | 95.8 |
| - | Civil servant | 26 | 4.2 |
| Mother’s education | Elementary school | 76 | 12.3 |
| - | Junior high school | 75 | 12.1 |
| - | Senior high school | 354 | 57.2 |
| - | Higher education | 114 | 18.4 |
| Mother’s occupation | Non-civil servant | 597 | 96.4 |
| - | Civil servant | 22 | 3,6 |
| Family type | Non-nuclear family | 59 | 9.5 |
| - | Nuclear family | 560 | 90.5 |
| Family income | < Regional minimum wage (Rp.4,642,000.00) | 384 | 62.0 |
| - | ≥ Regional minimum wage (Rp.4,642,000.00) | 235 | 38.0 |
| Socioeconomic environmental status | Poor | 28 | 4.5 |
| - | Adequate | 295 | 47.7 |
| - | Good | 296 | 47.8 |
3.2. Outer Model Testing
Table 2 presents the results of convergent validity, reliability, and average variance extracted (AVE) testing using the PLS algorithm output. The loading factor (FL) values for all the sub-variables were > 0.70 (ranging from 0.875 for negative cognition [Y1.3] to 0.983 for self-control [X3.3]). The AVE values were > 0.50 (ranging from 0.821 for adolescent resilience [Y1] to 0.953 for external risk factors [X2]). Therefore, each sub-variable and variable in the research model’s instrument met the requirements for convergent validity.
The individual protective factors (X3) sub-variable that most strongly determined the presence of HIV-AIDS prevention behavior (Y2) was self-control (X3.3; 0.983). Meanwhile, the weakest adolescent resilience (Y1) sub-variable was negative cognition (Y1.3; 0.875).
3.3. Internal Model Reliability and Discriminant Validity Testing
The results of the reliability testing of the research model are shown in Table 3. The SmartPLS output in the table indicates that all the constructs had Cronbach’s Alpha (CA) values ranging from 0.993 (external risk factors [X2]) to 0.974 (internal risk factors [X1]), rho_A values ranging from 0.994 (external risk factors [X2]) to 0.975 (internal risk factors [X1]), and Composite Reliability (CR) values ranging from 0.994 (external risk factors [X2]) to 0.978 (internal risk factors [X1]). Overall, the latent constructs had Cronbach’s alpha values exceeding 0.7, indicating good reliability. Therefore, it can be concluded that each sub-variable and variable in the present study had good reliability in measuring adolescent resilience (Y1) and HIV-AIDS prevention behavior (Y2).
| Variable | Sub-Variable | Construct | Convergent Validity | |
|---|---|---|---|---|
|
FL (> 0.70) |
AVE (> 0.50) |
|||
| Internal risk factors (X1) | Age | X1.1 | 0.910 | 0.845 |
| Sex | X1.2 | 0.916 | ||
| Ethnicity | X1.3 | 0.923 | ||
| Daily allowance | X1.4 | 0.902 | ||
| Living with family | X1.5 | 0.919 | ||
| Dating history | X1.6 | 0.937 | ||
| Duration of dating | X1.7 | 0.932 | ||
| Risky sexual behavior | X1.8 | 0.916 | ||
| External risk factors (X2) | Family type | X2.1 | 0.978 | 0.953 |
| Mother’s education | X2.2 | 0.973 | ||
| Father’s education | X2.3 | 0.976 | ||
| Mother’s occupation | X2.4 | 0.981 | ||
| Father’s occupation | X2.5 | 0.974 | ||
| Family income | X2.6 | 0.977 | ||
| Socioeconomic environmental status | X2.7 | 0,975 | ||
| Exposure to pornography from media | X2.8 | 0.977 | ||
| Individual protective factors (X3) | Coping strategy | X3.1 | 0.979 | 0.939 |
| Attitudes toward HIV-AIDS | X3.2 | 0.971 | ||
| Self-control | X3.3 | 0.983 | ||
| Knowledge about HIV-AIDS | X3.4 | 0.972 | ||
| Self-esteem | X3.5 | 0.936 | ||
| Self-efficacy | X3.6 | 0.973 | ||
| Sociocultural protective factor (X4) | Family resilience | X4.1 | 1.000 | 1.000 |
| Adolescent resilience (Y1) | Self-confidence | Y1.1 | 0.916 | 0.821 |
| Emotional insight/awareness | Y1.2 | 0.917 | ||
| Negative cognition | Y1.3 | 0.875 | ||
| Social skills | Y1.4 | 0.928 | ||
| Empathy | Y1.5 | 0.919 | ||
| Family attachment | Y1.6 | 0.917 | ||
| Family presence/existence | Y1.7 | 0.891 | ||
| Friend attachment | Y1.8 | 0.877 | ||
| Friend presence/existence | Y1.9 | 0.917 | ||
| School environment | Y1.10 | 0.903 | ||
| School attachment | Y1.11 | 0.913 | ||
| Community attachment | Y1.12 | 0.899 | ||
| HIV-AIDS prevention behavior (Y2) | HIV-AIDS prevention behavior | Y2.1 | 1.000 | 1.000 |
| Variables | Internal Consistency Reliability | Discriminant Validity (Heterotrait-Monotrait Ratio) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| - |
CA (> 0.70) |
rho_A (> 0.70) |
CR (> 0.70) |
X1 | X2 | X3 | X4 | Y1 | Y2 |
| X1. Internal risk factors (X1) | 0.974 | 0.975 | 0.978 | - | - | - | - | - | |
| X2. External risk factors (X1) | 0.993 | 0.994 | 0.994 | 0.101 | - | - | - | - | |
| X3. Individual protective factors | 0.987 | 0.988 | 0.989 | 0.753 | 0.187 | - | - | - | |
| X4. Sociocultural protective factor | 1.000 | 1.000 | 1.000 | 0.609 | 0.143 | 0.633 | - | - | |
| Y1. Adolescent resilience | 0.980 | 0.981 | 0.982 | 0.755 | 0.059 | 0.727 | 0.747 | - | |
| Y2. HIV-AIDS prevention behavior | 1.000 | 1.000 | 1.000 | 0.829 | 0.024 | 0.779 | 0.750 | 0.895 | |
Based on the results of the heterotrait-monotrait ratio (HTMT) testing regarding the correlations of all the variables in the questionnaire, all the dimensions had < 0.90 (0.024–0.895) values. Thus, the questionnaire met the criteria for discriminant validity in measuring adolescent resilience (Y1) and HIV-AIDS prevention behavior (Y2).
3.4. Structural Model Testing (Inner Model)
The R2 values can are shown in Fig. (2) and Table 4. The individual protective factors variableis 0.562, which means that the internal and external risk factors simultaneously influence the individual protective factors by 56.2%. The sociocultural protective factors variableis 0.370, indicating that the internal and external risk factors simultaneously influence the sociocultural protective factor by 37%. The adolescent resilience variable is 0.734, implying that the internal and external risk factors simultaneously influence adolescent resilience through the individual and sociocultural protective factors by 73.4%. Finally, for the HIV-AIDS prevention behavior variable, it is 0.871, meaning that the internal and external risk factors simultaneously influence adolescent resilience through individual protective factors, sociocultural protective factors, and adolescent resilience by 87.1%. This suggests that all the five variables measuring HIV-AIDS prevention behavior (X1, X2, X3, X4, and Y1) collectively have an influence of 87.10, categorized as a significant impact (> 67.00%), and the remaining 12.90% is influenced by other variables outside the research model.
Regarding the effect sizes of all the variables based on ƒ-square as shown in Table 4, an effect size > 0.02 is considered small, > 0.15 is medium, and > 0.35 is large. The variable that measures HIV-AIDS prevention behavior (Y2) most strongly is adolescent resilience (Y1), with an ƒ-square value of 0.369 (large). On the other hand, the variable that measures HIV-AIDS prevention behavior (Y2) most weakly is external risk factors (X2), with an ƒ-square value of 0.051 (small).
The predictive relevance Q2 (redundancy) results in Table 4 show Q2 values ranging from 0.367 (sociocultural protective factor) to 0.865 (HIV-AIDS prevention behavior). These Q2 values are greater than 0, indicating strong predictive relevance. Therefore, the model in the present study can explain 36.70–86.50% of observed phenomena, meaning that the observed values have been well reconstructed, and the model has predictive relevance. The Q2 (communality) values indicate strong predictive power for all the six variable dimensions, ranging from 0.781 (adolescent resilience) to 0.931 (external risk factors).
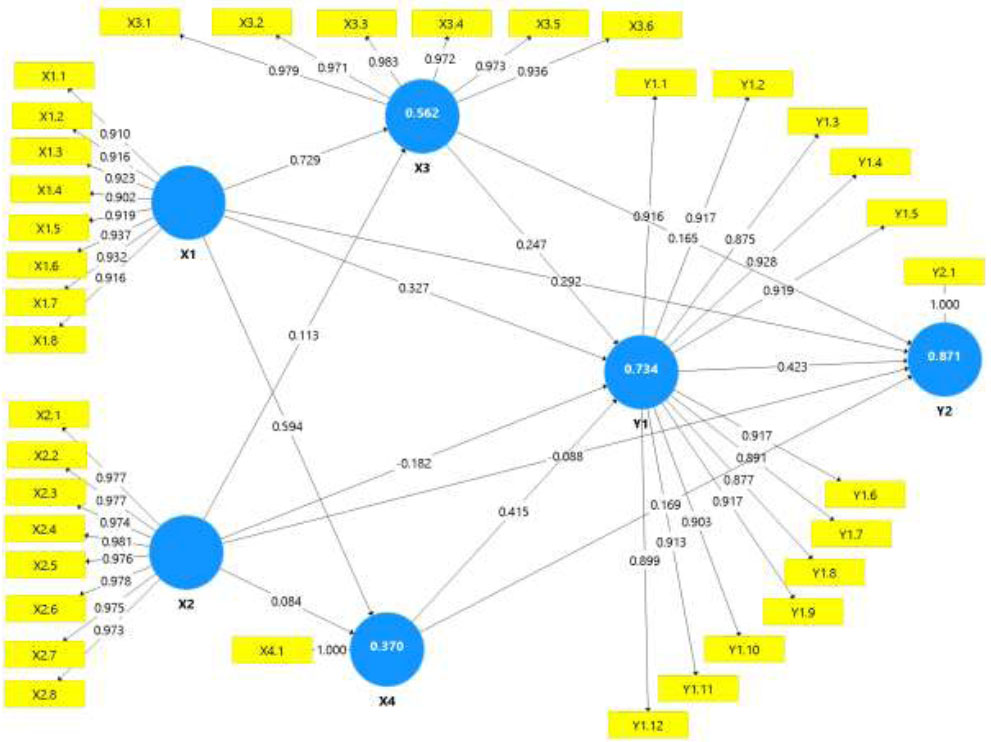
Structural model testing (inner model).
| Variables | R2 | Effect Size (ƒ-square) | Predictive Relevance (Q2) | |||||
|---|---|---|---|---|---|---|---|---|
| Value & Decision | Value & Decision | SSO | Redundancy | - | - | Predictive Power | ||
| SSE | Q2 (1-SSE/SSO) | SSE | Q2 (1-SSE/SSO) | |||||
| > 0.35 | >0,35 | |||||||
| X1. Internal risk factors | - | 0.236 (Medium) | 4952,000 | 4952,000 | - | 1025,214 | 0,793 | Strong |
| X2. External risk factors | - | 0.051 (Small) |
4952,000 | 4952,000 | - | 342,669 | 0,931 | Strong |
| X3. Individual protective factors | 0.562 (Moderate) |
0.075 (Small) | 3714,000 | 1766,980 | 0,524 | 346,710 | 0,907 | Strong |
| X4. Sociocultural protective factor | 0.370 (Moderate) | 0.091 (Small) |
619,000 | 391,619 | 0,367 | - | 1,000 | Strong |
| Y1. Adolescent resilience | 0.734 (Substantial) | 0.369 (Large) | 7428,000 | 2979,334 | 0,599 | 1628,834 | 0,781 | Strong |
| Y2. HIV-AIDS prevention behavior | 0.871 (Substantial) | - | 619,000 | 83,778 | 0,865 | - | 1,000 | Strong |
The calculated Q2 value of 0.865 indicates the relative influence of the structural model on the measurement of observations for endogenous latent variables, with a 13.5% model error. The predictive relevance test results (Q2) show that the model for measuring adolescent resilience (Y1) and HIV-AIDS prevention behavior (Y2) has strong predictive power (Q2 > 0.35).
3.5. Hypothesis Testing
In Table 5, the influences of adolescent resilience and HIV-AIDS prevention behavior are significant and positively directed. However, the influence of internal risk factors on adolescent resilience and the influence of external risk factors on HIV-AIDS prevention behavior were significant but negatively directed. For example, in hypothesis H8.1 (external risk factors [X2] → HIV-AIDS prevention behavior [Y2]), the β-value was -0.088 (negative decimal), the t-statistic was 6.127 (> 1.96), and the p-value was 0.000 (< 0.05), indicating that external risk factors (X2) have significant and negative influences on HIV-AIDS prevention behavior (Y2). This implies that an increase in the external risk factors (X2) would lead to a decrease in HIV-AIDS prevention behavior (Y2) and vice versa.
The most significant and positive influence on HIV-AIDS prevention behavior (Y2) is from adolescent resilience (Y1), with a β-value of 0.423. This is followed by internal risk factors (X1), which have a positive impact, with a β-value of 0.292; sociocultural protective factor (X4), with a β-value of 0.169; and individual protective factors (X3), with a β-value of 0.165. The smallest impact is from external risk factors (X2), with a β-value of -0.088, indicating a negative effect.
In Table 6, there are 12 indirect influence paths whose scores are significant in describing indirect effects through one mediator variable, namely adolescent resilience (Y1), which can be seen from the coefficient value on each path. For H-IND5 (“Adolescent resilience [Y1] significantly moderates the relationship between internal risk factors [X1] and HIV-AIDS prevention behavior [Y2] in high school students”), the results of testing the moderation effect of adolescent resilience (Y1) between internal risk factors (X1) and HIV-AIDS prevention behavior (Y2) suggest a positive and significant moderation effect (β-value = 0.138; t-statistic = 8.174 > 1.96; p = 0.000 < 0.05). Thus, H-IND5 was accepted. This suggests that the mediating role of adolescent resilience (Y1) is crucial for enhancing the impact between internal risk factors (X1) and HIV-AIDS prevention behavior (Y2).
For H-IND6, adolescent resilience (Y1) was shown to have a negative (an increase in external risk factors leads to a decrease in HIV-AIDS prevention behavior), and the effect is a statistically significant moderating effect (β-value = -0.077) on the relationship between external risk factors (X2) and HIV-AIDS prevention behavior (Y2) (t-statistic = 8.242 > 1.96; p = 0.000 < 0.05). H-IND6 (“There is a significant influence between external risk factors [X2] and adolescent resilience (Y1) to enhance HIV-AIDS prevention behavior [Y2] in high school students”) is also accepted. This suggests that the mediating role of adolescent resilience (Y1) is necessary to decrease the negative impact of external risk factors (X2) on HIV-AIDS prevention behavior (Y2).
The study also showed an indirect effect for H-IND8, the results of testing the moderation effect of the adolescent resilience (Y1) have a positive (β-values = 0.105) and significant impact (T-value 5.937 >1.96 and ρ-values = 0.000 < 0.05) between individual protection factors (X3) on HIV-AIDS prevention behavior (Y2). For H-IND11, adolescent resilience (Y1) was shown to have a positive and significant moderating effect (β-values = 0.176) between sociocultural protection factors (X4) and HIV-AIDS prevention behavior (Y2) (T-value 8.681 >1.96 and ρ-values = 0.000 < 0.05). Based on these results, H-IND8 and H-IND11 (“There is a significant influence between individual protection factors [X3] and adolescent resilience [Y1] to enhance HIV-AIDS Prevention Behavior [Y2] in high school students”) and H-IND11 (“There is a significant influence between sociocultural protection factors [X4] and adolescent resilience [Y1] to enhance HIV-AIDS Prevention Behavior [Y] in high school students”) was accepted. In conclusion, the mediating role of the adolescent resilience variable (Y1) is needed to increase the positive effect of the individual protection factors (X3) and sociocultural protection factors (X4) on HIV-AIDS prevention behavior (Y2).
| Hypothesis | Path Analysis | β-value* | T-statistic | P-value | Result | Conclusion |
|---|---|---|---|---|---|---|
| (+/-) | (> 1.96) | (< 0.05) | ||||
| H1.1 | X1. Internal risk factors → X3. Individual protective factors | 0.729 | 31.358 | 0.000 | Positive, significant | Hypothesis accepted |
| H2.1 | X1. Internal risk factors → X4. Sociocultural protective factor | 0.594 | 22.326 | 0.000 | Positive, significant | Hypothesis accepted |
| H3.1 | X1. Internal risk factors → Y1. Adolescent resilience | 0.327 | 10.357 | 0.000 | Positive, significant | Hypothesis accepted |
| H4.1 | X1. Internal risk factors → Y2. HIV-AIDS prevention behavior | 0.292 | 10.903 | 0.000 | Positive, significant | Hypothesis accepted |
| H5.1 | X2. External risk factors → X3. Individual protective factors | 0.113 | 3.606 | 0.000 | Positive, significant | Hypothesis accepted |
| H6.1 | X2. External risk factors → X4. Sociocultural protective factor | 0.084 | 2.280 | 0.023 | Positive, significant | Hypothesis accepted |
| H1.1 | X2. External risk factors → Y1. Adolescent resilience | -0.182 | 10.438 | 0.000 | Negative, significant | Hypothesis accepted |
| H8.1 | X2. External risk factors → Y2. HIV-AIDS prevention behavior | -0.088 | 6.127 | 0.000 | Negative, significant | Hypothesis accepted |
| H9.1 | X3. Individual protective factors → Y1. Adolescent resilience | 0.247 | 7.575 | 0.000 | Positive, significant | Hypothesis accepted |
| H10.1 | X3. Individual protective factors → Y2. HIV-AIDS prevention behavior | 0.165 | 4.795 | 0.000 | Positive, significant | Hypothesis accepted |
| H11.1 | X4. Sociocultural protective factor → Y1. Adolescent resilience | 0.415 | 12.434 | 0.000 | Positive, significant | Hypothesis accepted |
| H12.1 | X4. Sociocultural protective factor → Y2. HIV-AIDS prevention behavior | 0.169 | 7.018 | 0.000 | Positive, significant | Hypothesis accepted |
| H13.1 | Y1. Adolescent resilience → Y2. HIV-AIDS prevention behavior | 0.423 | 12.129 | 0.000 | Positive, significant | Hypothesis accepted |
| Hip. | Path Analysis | β-value* | T-statistic | P-value | Result | Conclusion |
|---|---|---|---|---|---|---|
| (+/-) | (> 1.96) | (< 0.05) | ||||
| H-IND1 | X1 -> X3 -> Y2 | 0.120 | 4.918 | 0.000 | Positive, significant | Hypothesis accepted |
| H-IND2 | X2 -> X3 -> Y2 | 0.019 | 2.724 | 0.007 | Positive, significant | Hypothesis accepted |
| H-IND3 | X1 -> X4 -> Y2 | 0.101 | 6.693 | 0.000 | Positive, significant | Hypothesis accepted |
| H-IND4 | X2 -> X4 -> Y2 | 0.014 | 2.304 | 0.022 | Positive, significant | Hypothesis accepted |
| H-IND5 | X1 -> Y1 -> Y2 | 0.138 | 8.174 | 0.000 | Positive, significant | Hypothesis accepted |
| H-IND6 | X2 -> Y1 -> Y2 | -0.077 | 8.242 | 0.000 | Negative, significant | Hypothesis accepted |
| H-IND7 | X1 -> X3 -> Y1 -> Y2 | 0.076 | 5.740 | 0.000 | Positive, significant | Hypothesis accepted |
| H-IND8 | X3 -> Y1 -> Y2 | 0.105 | 5.937 | 0.000 | Positive, significant | Hypothesis accepted |
| H-IND9 | X2 -> X3 -> Y1 -> Y2 | 0.012 | 2.819 | 0.005 | Positive, significant | Hypothesis accepted |
| H-IND10 | X1 -> X4 -> Y1 -> Y2 | 0.104 | 8.343 | 0.000 | Positive, significant | Hypothesis accepted |
| H-IND11 | X4 -> Y1 -> Y2 | 0.176 | 8.681 | 0.000 | Positive, significant | Hypothesis accepted |
| H-IND12 | X2 -> X4 -> Y1 -> Y2 | 0.015 | 2.195 | 0.029 | Positive, significant | Hypothesis accepted |
4. DISCUSSION
This study confirmed all 13 direct hypotheses and 12 indirect hypotheses, demonstrating that internal and external risk factors, as well as individual and socio- cultural protective factors, influence adolescent resilience in preventing HIV infection. Internal risk factors were also shown to affect individual protective factors.
Our results indicate that adolescents employ various coping strategies depending on stress triggers, with no significant gender difference observed [45-47]. Problem-focused coping, particularly enhancing problem-solving skills, was predominant. Self-esteem mediates the relationship between coping and depression reduction [48]. While a study [49] reported male and female adolescents in the coping strategies, they found no significant influence of gender on self-efficacy.
Regarding self-efficacy, Kisaaayke et al. [50] reported noted lower levels among girls, often due to their communication weakness, reluctance to refuse their partners’ condom use (57.2% were afraid to refuse), or fear of asking their partners to use condoms (4.4% were afraid). In addition, 53% of the male adolescents in their study could not maintain self-efficacy in their sexual relationships for 12 months, while the young female adolescents were able to maintain it(PR = 0.69; 95% CI = 0.48, 1.02). Self-esteem showed no significant gender difference in relation to risky sexual behavior [51], but 11- to 19-year-old female adolescents tended to develop resilience [42, 52, 53]. Ethnicity was found to moderate the relationship between racism and self-blame, negatively impacting adolescent resilience [54].
Internal factors, such as adolescent’s pocket money, can influence their use of condoms during sexual intercourse as HIV-AIDS prevention behavior [55]. Adolescents with a large amount of pocket money were at risk of engaging in risky sexual behavior, such as buying credit to access pornographic films online [34]. These findings differ from those of studies on adolescents with little pocket money, who were shown to be at a higher risk of engaging in transactional sex to meet their needs [56, 57]. Thus, internal factors influence HIV-AIDS prevention behavior.
Research by Pengpid & Peltzer [58] has shown that male adolescents among 15- to 19-year-olds indicated a higher prevalence of HIV cases due to their aggression and strong sexual desire. This behavior consequently increases HIV transmission to female adolescents [59-61]; especially those in urban areas [62-64].
Shanaube et al. [65] found that internalization issues (e.g., low self-esteem, depression, and anxiety) were related to low self-efficacy, decreased assertiveness, and a lack of ability to negotiate safe sex. This is supported by the results of the Kurniyawan et al. [66] study, in which 84 adolescent respondents had moderate self-efficacy (46.4%), and a significant relationship was shown between parenting style, lifestyle, and self-efficacy in preventing HIV-AIDS (p = 0.026). In Zakiei et al.’s. Research involving 765 subjects (59% female) [67] emphasized the key role of self-efficacy in HIV-AIDS prevention behavior.
Dating history and duration were identified as internal risk factors, affecting overly close and open social relationships [68], potentially leading to premarital sexual behavior [10], and affecting psychological health and adolescent resilience [69]. Keto et al. [55] reported high rates of multiple sexual partners and inconsistent condom use among adolescents.
Furthermore, adolescents with external risk factors, such as low socioeconomic status (e.g., those whose families have wages below the minimum wage), were associated with low resilience and a higher risk of STI and HIV infection [70]. Family socioeconomic status, including parental education, occupation, income, and family type and function, affects adolescent resilience and HIV-AIDS prevention behavior [71]. Exposure to pornography was linked to risky sexual behavior and externalization of problems, especially rule violations and aggressive behavior [72]. Approximately 50% of adolescents are significantly exposed to explicit sexual media, increasing their early sexual debut, unsafe sexual relationships, and changing sexual partners [73]. Education on the proper sexual behavior in adolescents is thus needed.
Individual protective factors (e.g., self-control components, coping strategies, attitudes toward HIV-AIDS prevention, knowledge about HIV-AIDS, self-esteem, and self-efficacy) also influence HIV-AIDS prevention behavior. Esmaeilzadeh et al. [74] found that low self-control significantly increased condom use in sexual relationships, while high self-efficacy significantly increased the likelihood of condom use. It was also reported that 25.6% of the respondents in the same study engaged in unsafe sexual relationships with multi-sexual partners, and of these respondents, 22.5% had low self-control, and 4.7% had high self-control (X2 = 9.708; p = 0.002). Self-control influences HIV-AIDS prevention behavior the most.
Our study highlights the complex interplay of factors influencing adolescent resilience and HIV-AIDS prevention behavior. Adolescents’ coping strategies are pre- dominantly task-oriented (e.g., distraction/diversion with one’s parents and peers), with cognitive and active coping potentially fostering positive emotions [47, 75]. However, negative emotions and low self-esteem can increase the likelihood of risky sexual behavior [51]. Adolescents’ perceptions of self-efficacy can affect the levels of their psychological well-being and their success in preventing risky sexual behavior [76, 77]; thus, self-efficacy plays a key role in HIV-AIDS prevention behavior [67]. Compre- hensive interventions are therefore needed to improve individual protective factors in HIV-AIDS prevention programs for adolescents.
Knowledge about HIV-AIDS and attitudes toward HIV-AIDS prevention were significantly related to HIV-AIDS prevention behavior [78, 79]. Limited comprehensive knowledge was identified as a main factor in the high prevalence of HIV-AIDS among adolescents [22, 80, 81]. Students with higher knowledge about HIV-AIDS generally have a lower likelihood of engaging in risky sexual behavior because most of them have received health education about HIV-AIDS [82-84]. Implementing sexual health education programs was deemed crucial for enhancing HIV-AIDS prevention behavior [85, 86].
Sociocultural protective factors involve adolescents’ characteristics related to the role of the family that influence their risky sexual behavior [87, 88]. Students who live far from their biological parents show higher risk factors for sexual behavior [88, 89]. Sexual behavior in adolescents is strongly influenced by how families perform their roles and functions toward the adolescents in the family; thus, parental parenting patterns strongly influence sexual behavior [90]. Family resilience and family parenting activities play a crucial role in realizing adolescent resilience by improving family function [91-93]. The proper functioning of the family under the leadership of the parents can influence the behavior of the other family members; thus, family functioning affects adolescent resilience and behavior [94]. Increased adolescent resilience is related to HIV prevention behavior, as evidenced by increased health-promoting behavior in risky groups affected by HIV, such as compliance with antiretroviral consumption and support from peers [85].
Resilience is generally defined only at the individual level (psychological) and most studies focus on limited individual and interpersonal resilience (e.g., social support). A multi-system model of resilience approach is needed to better represent the resilience construct, including individual—especially adolescent—interpersonal and environmental resilience steps is thus needed [95, 96]. Govender et al. [97] emphasized that the promotion and maintenance of HIV prevention requires an effective cross-sector partnership with a regional vision and a process led by countries made possible through strong participation and accountability from all stakeholders. Community resources that support it, including teachers, peers, adult mentors, and school personnel, are essential in forming adolescent resilience [98].
Adolescent resilience is a dynamic process involving adolescents adapting to pressures, stressors, and life challenges to achieve well-being. This process encompasses individual domains such as self-confidence, emotional awareness, negative cognition, social skills, and empathy/tolerance, and environmental domains such as family relationships, family access, peer communication, access to peers, academic support environments, academic communication, and communication with the community [99, 100]. Developing resilience through peer-based health education strategies can significantly influence emotional adjustment and adolescent resilience, thus offsetting the negative impacts of sexual issues on adolescents, especially before marriage [101, 102]. Health education for adolescents should also be engaging, employing strategies that are straightforward, communicative, and well-received by adolescents [103].
4.1. Nursing Implications
This study’s findings have significant implications for nursing practice, education, and research. Nurses play a crucial role in adolescent health promotion and HIV-AIDS prevention. They should incorporate resilience-building strategies into their interventions, focusing on enhancing self-efficacy, problem-solving skills, and positive coping mechanisms among adolescents. Nursing education programs should emphasize the importance of under- standing the complex interplay of risk and protective factors influencing adolescent health behaviors. Nurses should be trained to provide culturally sensitive, age-appropriate sexual health education and counseling. In community health settings, nurses can lead family-focused interventions to improve parent-adolescent communication about sexual health. School nurses are well-positioned to implement peer-based education programs and collaborate with teachers to integrate HIV-AIDS pre- vention into the curriculum. In research, nurses should contribute to the development and evaluation of innovative interventions that address both individual and socio- cultural factors affecting adolescent resilience and HIV-AIDS prevention behaviors.
4.2. Limitations
This study has several limitations that should be considered when interpreting the results. First, the cross-sectional design limits our ability to establish causal relationships between the factors studied and adolescent resilience or HIV-AIDS prevention behavior. Longitudinal studies would be beneficial to track changes over time and better understand the developmental aspects of resilience and prevention behaviors. Second, the study relied on self-reported data, which may be subject to social desirability bias, especially given the sensitive nature of topics related to sexual behavior and HIV-AIDS. Future research could benefit from incorporating more objective measures, or mixed-methods approaches to triangulate findings. Third, while our sample was representative of high school students in Jakarta, the results may be generalizable to adolescents in other regions of Indonesia but not to those who are not in school. Further studies should consider including a more diverse sample of adolescents from various geographical and socioeconomic backgrounds.
CONCLUSION
The results of the present study indicate that the factor that most significantly influences variables related to HIV-AIDS prevention behavior is adolescent resilience (β-value = 0.423; t-statistic = 12.129), followed by internal risk factors (β-value = 0.292; t-statistic = 10.903). External risk factors were observed to have the smallest influence (β-value = -0.088; t-statistic = 6.127), which was significantly negative. The sub-variable that most strongly or dominantly measures HIV-AIDS prevention behavior (Y2) is self-control (λ = 0.983), while the sub-variable that most weakly measures it is negative cognition (λ = 0.875). In conclusion, adolescent resilience is a key factor in improving HIV-AIDS prevention behavior among adolescents because it plays a significant role in influencing adolescent beliefs, boosting self-confidence, developing emotional insight, and fostering social skills and empathy toward others. It is thus crucial to enhance it in HIV-AIDS prevention programs.
The study’s findings can be applied to all Indonesian provinces because DKI Jakarta, as the country’s capital, represents all features of Indonesian high school and vocational school students. Additionally, the respondents’ ethnic backgrounds include those from the islands of Java as well as other islands such as Sumatra, Kalimantan, and Sulawesi.
AUTHORS' CONTRIBUTION
DR, AS, WW, TSU, SRA, study concept; DR, SPH, TS, data curation; DR, SPH, TS, formal analysis; DR, AS, WW, investigation; DR, AS, WW, SPH, methods, resources; DR, TS, software; AS, TSU, supervision; WW, SPH, SRA, validation; DR, AS, TS, original manuscript draft, review, and editing. All the researchers have read and approved the final version of the manuscript and agree to be accountable for all aspects of the research.
ABBREVIATION
| HIV | = Human Immunodeficiency Virus |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
These procedures have undergone ethical testing for health research by the Research Ethics Committee of the Faculty of Nursing, Depok, Indonesia (FIK UI No. KET-029/UN2.F12.D1.2.1/ PPM.00.02/2023).
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all respondents, and they were clearly informed that they could refuse to participate or withdraw from the study at any time without any consequences. This ensured that the students’ participation was based on their own free will.
AVAILABILITY OF DATA AND MATERIALS
There are no additional supporting data or repository entries for this study. All relevant data and supportive information are available within the article or upon request from the corresponding author [A.S].