All published articles of this journal are available on ScienceDirect.
Challenges in Insulin Therapy: Perspectives of Malaysian Diabetes Educators
Abstract
Background
Individuals with type 2 Diabetes Mellitus (T2DM) commonly need insulin therapy as their condition advances. Healthcare providers often face difficulties in managing patients who require insulin treatment. Gaining insight into the views of healthcare professionals on the obstacles encountered by patients using insulin can aid in improving care and developing effective treatment plans.
Objective
This study explores the views of Malaysian diabetes educators on the barriers faced by patients in using insulin.
Methods
Semi-structured qualitative interviews were conducted with diabetes educators (n=8) from the northern, central, and southern regions of Malaysia who were involved in diabetes care. We used an interview guide to facilitate the in-depth interviews, which were digitally recorded, transcribed verbatim, and analyzed using a thematic approach.
Results
Five themes were identified: the occurrence of side effects, the need for better patient education, negative perceptions towards insulin, the financial burden, and the complexity of adherence to treatment. There is a lack of patient education on proper glucose monitoring and how to optimize insulin therapy. The cost of treatment and patient ignorance are highlighted when discussing patient self-monitoring of blood glucose. Diabetes educators recognize that the absence of an effective follow-up mechanism is a major issue, particularly for those patients who fail to maintain consistent appointment schedules.
Conclusion
This research highlights five significant obstacles to maximizing the effectiveness of insulin therapy. Diabetes educators who identify and address these challenges can empower patients to manage their condition effectively. To overcome systemic barriers, government involvement is needed in creating insulin follow-up initiatives, establishing multidisciplinary teams for diabetes care, empowering education strategies, and providing financial support for self-monitoring.
1. INTRODUCTION
Diabetes mellitus (DM) is a prevalent, chronic, non-communicable disease that significantly contributes to disability and mortality worldwide [1]. According to the World Health Organization (WHO), almost 50% of people suffering from chronic disorders like T2DM do not adhere to their treatment [2].
The latest study reported the primary non-adherence factors, such as age, healthcare expenses, individual attitudes towards insulin therapy, societal discrimination, patient education, the intricacy of diabetes treatment, the consequences of insulin therapy on everyday activities, and apprehension of adverse effects [3]. When compared with users of oral antidiabetic medications, insulin users were found to have a significantly higher incidence of non-adherence due to its correlation with a greater number of physical and societal repercussions. Insulin is considered to have more significant implications [2].
Adherence can be defined as a person's behaviour, which in the context of this study reflects on patients' behaviours towards compliance with medication, following diet recommendations, changing lifestyle modifications, and having a mutual agreement between patients and healthcare workers [4]. In addition, adherence pertains to the extent to which an individual adheres to the prescribed medication regimen as prescribed by a health- care practitioner [5, 6].
In Malaysia, the glycaemic control of patients attending public hospitals was suboptimal [7]. The proportion of diabetic patients achieving optimal control was 13% in tertiary healthcare facilities and 24% in primary care facilities [8]. Statistics from an extensive study on Adult Diabetes Control and Management conducted across 303 centres and included 70,889 individuals with T2DM revealed that only 30.9% of the participants achieved an HbA1c level below 7.0% [9]. Most people with T2DM will eventually need insulin therapy as a more advanced approach to effectively managing their blood sugar levels. Patients with T2DM frequently exhibit resistance to medical recommendations for insulin therapy, primarily due to misconceptions about injectable medicine [10].
Low adherence to disease management has detrimental effects on various aspects, such as worsening conditions leading to acute hospitalizations, elevated healthcare expenses, and a notable decline in patients' quality of life [6]. The implementation of a multi- disciplinary approach from physicians, nurses, and educators has the potential to address issues and improve adherence among patients with T2DM to insulin therapy [11]. Through a holistic approach from the dedicated multidisciplinary team, the quality of diabetes treatment is enhanced, and insulin therapy is effectively facilitated among patients [10-12]. The utilization of interdisciplinary treatment teams may potentially emerge as the optimal approach for attaining favourable clinical outcomes in individuals diagnosed with diabetes. Numerous studies have consistently proved that the utilization of multidisciplinary teams leads to enhanced outcomes while also showcasing favourable or neutral impacts on costs [13]. However, despite knowing the effectiveness of insulin therapy in managing diabetes, adherence still remains a global issue. More research is needed to better understand the factors influencing insulin therapy adherence in Malaysia. Since diabetes educators in Malaysia are among the dedicated healthcare workers involved in managing diabetes, this study primarily explores their views on the barriers faced by patients in using insulin therapy.
2. MATERIALS AND METHODS
2.1. Design, Sample, and Setting
A qualitative descriptive study was conducted involving individual one-on-one interviews with diabetes educators from the northern, southern, central, east coast, Sabah, and Sarawak regions. This study is crucial in understanding the lived experiences of educators in managing patients with T2DM using insulin therapy. Eight states were involved in this study, and each state represented the regions and workplaces of diabetes educators.
To qualify for this group, participants were required to (1) be recognized as diabetes educators, (2) have completed a post-basic course certification from the Ministry of Health, (3) have clinical experience handling insulin patients with a minimum of one year, and (4) have internet access and email for interview purposes. This specific inclusion criteria ensured that the input gathered was from professionals well-versed in diabetes manage- ment, particularly in the nuances of insulin therapy. Meanwhile, individuals titled as diabetes educators but had not undergone formal certification from a Ministry-approved institutions were excluded.
2.2. Data Collection
The study started with receiving ethical approvals from multiple authoritative bodies, including the UiTM Ethics Committee and the Medical Research and Ethics Committee (MREC).
The process began by identifying diabetes educators across various Malaysian states. The participants were approached personally and screened for inclusion criteria. Once a participant met the criteria, the study was explained to them, and if they agreed, a consent form was provided. The participants' locations were categorized into regions: northern, southern, central, east coast, Sabah, and Sarawak, with each region represented by one diabetes educator. This categorization followed the establishment of inclusion criteria.
Due to constraints in coordinating focus group sessions and gathering the diabetes educator at one time, one-on-one interviews were conducted online and scheduled according to participant availability. These interviews typically lasted between 30 minutes and an hour. Conversations were recorded with the participants' acknowledgement that they would be used solely for research purposes. Upon completion of the data collection, an analysis was performed. This analysis transformed the collected data into results using thematic analysis [14-18].
Once data collection was completed, the textual data underwent multiple readings to facilitate the identification of themes and categories through a process termed “Persistence and Observation.” Multiple codes emerged, with relevant quotations systematically categorized under respective codes using ATLAS.ti Version 8 software. This process continued until reaching a saturation point, indicating that no additional themes were emerging, a principle referred to as 'Data Triangulation.'
2.3. Research Instrument
An interview guide for qualitative research is a methodical approach to conducting interviews that balances structure with the flexibility to explore participants' perspectives deeply [19]. The list of questions was developed based on the objective and literature following the Consolidated Criteria for Reporting Qualitative Research (COREQ) for making an interview protocol guide [19].
The interview guide of this research was systematically divided into two key sections. Section A was dedicated to gathering demographic data, including age, gender, educational qualifications, and professional experience of diabetes educators [19]. Meanwhile, section B comprised semi-structured, in-depth interview questions carefully formulated to understand the practical realities diabetes educators encounter in clinical settings, particularly during health education sessions for insulin therapy.
2.4. Ethical Considerations
Participants were informed about the study, including voluntary participation, and that any photographs or audio recordings would remain confidential and solely used for research purposes. Ethical approval was received from UiTM ethics committees, with approval numbers 18/7/2022(REC/07/2022(PG/FB/16)). Then, the researchers proceeded with the Malaysian National Medical Research Register's ethical applications, with the approval of the ethical number NMRR ID-22-00862-UHA.
3. RESULTS
3.1. Characteristics of Participants
The demographic details of the participants are summarized in Table 1. The participants consisted of eight diabetes educators, seven female and one male, with an age range of 29 to 45 years and a mean age of 35.7 years. Their experience in diabetes education and management spanned from 7 to 12 years. Notably, most of these educators engaged in direct contact with diabetes clients over 80% of the time.
3.2. Findings
Findings show data presented according to the major theme and subthemes in identifying the challenges of insulin therapy. Five major themes have been coded: (1) integrated education elements, (2) benefits of education, (3) challenges of insulin education, (4) psychological approaches, and (5) the role of diabetes educators in insulin education. The summary mapping of the major theme and subtheme is illustrated in Fig. (1).
3.2.1. Theme 1: Side Effects of Insulin Therapy
This study highlights the common side effects of insulin therapy in patients with T2DM, as noted by diabetes educators, with one key subtheme.
3.2.1.1. Subtheme 1.1: Risk of Hypoglycemia Complications
Participants found hypoglycaemia as one of the major issues in dealings with insulin therapy patients. As expressed by a diabetes educator:
Kesuma said: “For my elderly patients, the risk of hypoglycaemia is much higher than I need to explain the timing, dose, and education for physical exercises when they (patients) using insulin”.
Another participant said: “A lot of issues to educate them (patients), especially elderly had frequent hypoglycaemia episode during the physical exercises because they (patients) inject insulin and do high-intensity exercise” (Melur).
Participants also felt that insulin caused them (patients) to feel hungry, causing them to overeat, hence raising their blood sugar levels. They (patients) skip meals and induce hypoglycaemia. As expressed by diabetes educator:
“Compare when they use insulin, it makes them eat. They feel that after using insulin, the blood sugar goes even higher...then patients skip a meal and develop hypoglycaemia.” (Lily).
| Pseudonym* | Age | Gender | Qualification | Post Basic Course | Experience in Diabetes Education and Management |
Direct Contact with Diabetes Clients (% of total client load per month) |
|---|---|---|---|---|---|---|
| Alex | 35 | Male | BSc. Nursing | Certificate in Diabetes Management | 11 | 80 |
| Ros | 37 | Female | Dip. Nursing | Certificate in Diabetes Management | 10 | 90 |
| Mawar | 35 | Female | Dip. Nursing | Certificate in Diabetes Management | 7 | 100 |
| Kemboja | 38 | Female | Dip. Nursing | Certificate in Diabetes Management | 6 | 85 |
| Lily | 29 | Female | Dip. Nursing | Advanced Diploma in Diabetes Care | 6 | 100 |
| Melur | 45 | Female | BSc. Nursing | Advanced Diploma in Diabetes Care | 6 | 100 |
| Kesuma | 36 | Female | Dip. Nursing | Certificate in Diabetes Management | 11 | 90 |
| Melati | 36 | Female | BSc. Nursing | Certificate in Diabetes Management | 12 | 85 |
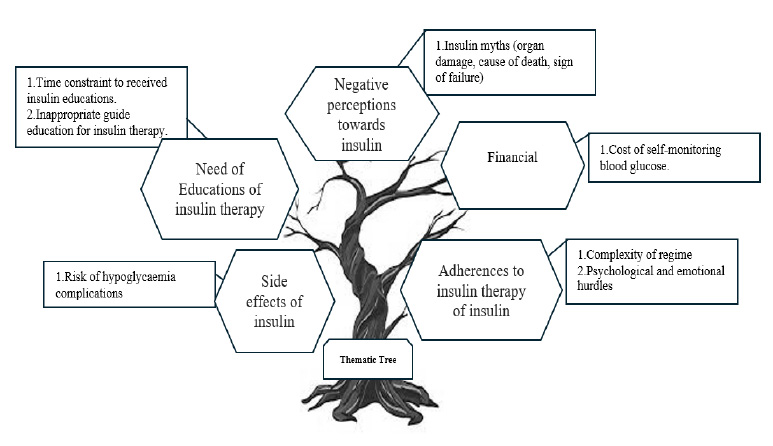
Thematic tree.
3.2.2. Theme 2: Need of Education
This theme elucidates the overview of insulin education in managing patients with diabetes. Two significant subthemes emerged under this theme.
3.2.2.1. Subtheme 2.1: Time Constraint to Receive Insulin Education
Time constraints to receive education regarding insulin therapy adherence show challenges in real clinical settings. As expressed by diabetes educator:
Participant Alex said: “They missed their appointment but still have a considerable supply of insulin...”
Another participant supported him: “I'm unable to modify the insulin dosage due to their lack of adherence to the treatment plan…. It's often frustrating to see persistent high HbA1c level…hmm” (Kesuma).
Lily said: “It’s our role to continuously motivate and support them…compliances to the treatment...hmm not easy, but we must help them…”.
Supported by Kemboja: “Adherences issued poor among insulin compared to oral medications...”.
Alex stated: “Sometimes we just need time to explore more about them…” Another participant said: “Our patients come with multiple backgrounds and needs, sometimes we can’t handle everything...” (Ros).
3.2.2.2. Subtheme 2.2: Inappropriate Guide Education for Insulin Therapy
Some patients with T2DM with insulin use need education on diabetes complications, including diabetes management, to improve their knowledge and skills. As expressed by diabetes educator:
Participant Ros said: My patient thought exercises were only for young patients…. She (elderly) never performs exercises since starting insulin due to afraid of hypoglycaemia…”
Another participant said: “My patient came to me, cried because the doctor suggested amputating her leg and plan for dialysis... she said because not received enough education for prevention measure...” (Melur).
Education material on insulin is limited, and diabetes educators jot down the information on blank papers. As expressed by diabetes educator:
Lily said: “I got used to making sketches and drawing to put all details on blank paper...” (Kesuma).
Another participant said: ” … our patients understand all the information, even my drawing is bad (laugh)...” (Alex).
3.2.3. Theme 3: Financial Burden
This theme illustrated the financial challenges of insulin therapy. One significant subtheme emerged in this context.
3.2.3.1. Subtheme 3.1: Financial Burden of Blood Glucose Monitoring
Poor control of blood sugar levels was also linked to poor adherence among participants about their diseases. This gap in understanding stemmed from challenges associated with self-monitoring blood glucose (SMBG) due to economic constraints. As expressed by diabetes educator:
“...They (patients) need to wait for salary to buy strips and all…” (Alex).
Another participant said, “Sometimes they (patients) simply check without knowing the pre and post-meal considerations…the cost of strips and all just wasted...” (Kesuma).
3.2.4. Theme 4: Negative Perceptions towards Insulin
This theme illustrated the challenges of insulin therapy in terms of patients' thoughts and perceptions. One significant subtheme emerged in this context. Diabetes educators identified negative perceptions that caused patients to discontinue insulin usage.
The diabetes educator stated that patients thought insulin was dangerous and could cause death. Patients also thought their diabetes would worsen after initiating the insulin. As a result, patients perceived that insulin was the reason for their diabetes complications. As expressed by diabetes educator:
“They (patient) thought once start insulin ...soon they (patient) will die...” (Mawar).
Another participant said: ‘... some patients will ask us, “Nurses, if I use insulin, soon I need to prepare for dialysis” (Lily).
According to a diabetes educator, one of the reasons patients have poor adherence is the stigma towards insulin.
“They (patient) ashamed with insulin…thought insulin makes them (patient) different from other communities…”. As stated by Alex: “My patients left insulin when attending feast...”.
3.2.5. Theme 5: Adherence to Insulin Therapy
This theme illustrates two subthemes regarding the challenges of adherence to insulin therapy.
3.2.5.1. Subtheme 5.1: Adherence to Insulin Therapy
Diabetes educators claim that patients have to comply with insulin therapy due to the complexity of the regime. According to diabetes educators, patients perceived insulin as a complex task and a reason to delay initiating therapy.
As stated by one of the participants:
“… without knowledge and guide... most of them (patients) drop insulin due to multiple excuses...” (Kesuma).
One participant described that the work routine makes it difficult for patients to comply with the meal and insulin regime.
“Some patients need to inject four times per day. One of my patients said she always has meetings outside, and the lunchtime is not consistent. She needs to follow her boss's schedule. She cannot bring an insulin pen 24 hours with her...” (Alex).
Meanwhile, another participant claimed: “He cannot comply with the four insulin per day. He is a teacher...” (Kesuma).
3.2.5.2. Subtheme 5.2: Psychological and Emotional
Participants attributed their (patients) suboptimal glucose management to personal issues, leading to feelings of anxiety, stress, and sadness. These emotional states prompted some individuals to engage in unhealthy eating behaviours and neglect their diabetes management routines, including the omission of insulin and other diabetes medications. As expressed by diabetes educator:
“They start crying when we explain the consequences of their action to their beloved person. Family? Son...? … They (patient) struggle to find the money for family but forget to take care of their health…” (Lily).
Another participant said: “… it’s not easy, and they (patient) stress…” (Alex).
Participants mentioned the complexity of the treatment and how emotional imbalance affects compliance with the treatment. Patients need to be assessed for their mental health status, especially among those with poor glycemic levels. As expressed by diabetes educator:
Kemboja said: “I had depressed patients; she is a single mother, and her HbA1c is 15.8 ...”.
Another participant said: “They can’t sleep over three months because the doctor said they want to start insulin on the next appointment...” (Kemboja).
4. DISCUSSION
The findings of the current study showed that patients faced multiple challenges while using insulin therapy from the perspective of diabetes educators. The biggest issue patients encounter is the challenge of adapting insulin therapy into their daily routine [20]. Some of the respondents expressed emotional burdens due to difficulties managing diabetes, especially insulin injection time and working schedules. It has been concluded from the patient's point of view that insulin therapy faces a number of challenges.
A study discovered that the major facilitators of insulin treatment were its relative effectiveness and convenience. These key facilitators include fewer gastrointestinal side effects, a smaller needle size, and ease of use [21]. In addition, patients cherished that insulin is a life-sustaining medication, had confidence in the decisions made by their physicians, had the support of their families, and benefited from health insurance coverage. However, the most common obstacles were market failures, such as the extremely high cost of insulin and supply shortages of insulin, as well as the characteristics of insulin and the conditions of patients [22]. The findings of this study are similar to those of the previous study, reporting that the cost of insulin is one of the challenges for insulin patients [23]. Recent studies have illuminated significant psychological hurdles in managing insulin therapy for diabetes patients, emphasizing the pervasive impact of these challenges on treatment efficacy. One prominent issue is the fear of hypoglycemia, where patients' anxiety over potential low blood sugar episodes can lead to counterproductive behaviors, such as overconsumption of carbohydrates or reluctance to adjust insulin dosages appropriately. Additionally, many patients experience a sense of burden and frustration due to the constant need for blood glucose monitoring and insulin administration, which can contribute to diabetes distress. This distress often includes feelings of helplessness, fear of complications, and anxiety about the social implications of their condition. Addressing these psychological barriers is crucial for improving adherence to insulin regimens and overall diabetes management outcomes [24]. Therefore, a mental health assessment is essential to promote better outcomes in diabetes management [25].
In some regions with limited affordable healthcare, insulin and accompanying supplies can be too expensive for some people [26]. Insulin therapy requires not only the medication itself but also various ancillary supplies, such as syringes, needles, insulin pens, blood glucose meters, and test strips. These items, when added to the already high cost of insulin, can become prohibitively expensive for patients without adequate health insurance or financial resources. As a result, individuals in these regions may be forced to ration their insulin or forego other essential diabetes management practices, leading to poor glycemic control and an increased risk of diabetes-related complications. The financial strain can also exacerbate psychological stress, as patients worry about their ability to afford the next dose of insulin or necessary supplies. This economic burden highlights the critical need for policies and programs that improve the affordability and accessibility of diabetes care, ensuring that all patients have the resources they need to manage their condition effectively.
To address these challenges, education plays a crucial role. Providing comprehensive education on diabetes management can empower patients to make informed decisions about their health. This includes teaching patients about cost-effective strategies, such as proper storage and handling of insulin to reduce waste and the importance of consistent monitoring to prevent costly complications [27]. Additionally, education programs can inform patients about available resources and assistance programs that can help reduce costs. Training healthcare providers to deliver culturally and regionally appropriate education can further enhance patient’s understanding and adherence [28]. By equipping patients with knowledge and practical skills, education can mitigate some of the financial and psychological burdens associated with diabetes management in resource-limited settings, ultimately improving health outcomes.
These problems highlight the need for comprehensive diabetes education, mental health support, and a robust support structure to help patients navigate insulin therapy and improve their quality of life [28]. Therefore, motivation and empowerment help patients adapt to the challenges, as diabetes patients, especially those addressing the emotional burden of diabetes, may improve adherence to treatment and self-care practices [29]. Diabetes management often requires significant lifestyle changes and constant vigilance, which can lead to emotional stress, anxiety, and even depression. The implementation of behaviour-change interventions can address these psychological factors, which significantly impact a person's ability to adhere to their treatment plan [30].
CONCLUSION
This study emphasizes the challenges faced by Type 2 Diabetes Mellitus (T2DM) patients undergoing insulin therapy, highlighting fears, misconceptions, and side effects that can impede effective self-management. It underscores the crucial role of healthcare providers, particularly diabetes educators, in overcoming these barriers by providing clear and comprehensive education about insulin therapy, dispelling myths, addressing patient fears, and advocating for support systems and regular follow-ups to monitor progress.
Furthermore, this study found that addressing emotional hurdles is important for managing adherence, particularly with insulin therapy, and highlighted that the assessment of mental health is crucial for improving adherence among patients. Organizationally, the integration of multidisciplinary diabetes care teams comprising endocrinologists, primary care physicians, nurses, dietitians, and diabetes educators can ensure coordinated and holistic patient care to enhance insulin adherence.
From a policy perspective, government initiatives should focus on establishing comprehensive insulin follow-up programs, providing financial support for essential diabetes management tools like glucometers and test strips, and promoting continuous professional develop- ment for diabetes educators to improve patient’s education and support. By addressing these recommen- dations, the self-management capabilities of T2DM patients on insulin therapy can be significantly improved, leading to better treatment adherence and an enhanced quality of life.
AUTHORS’ CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| NCD | = Non-Communicable Disease |
| T2DM | = Type 2 Diabetes Mellitus |
| ADA | = American Diabetes Association |
| WHO | = World Health Organization |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval was received from UiTM ethics committees, with approval numbers 18/7/2022(REC/ 07/2022(PG/FB/16)). The researchers proceeded with the Malaysian National Medical Research Register's ethical applications, with the approval of the ethical number NMRR ID-22-00862-UHA, Malaysia.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT TO PARTICIPATE
Each participant signed an informed consent before participating in this study.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.