All published articles of this journal are available on ScienceDirect.
Exploring Factors Influencing Posttraumatic Growth Among Nurses: A Path Analysis
Abstract
Introduction
Persistent exposure to the COVID-19 pandemic has subjected frontline nurses to heightened levels of collective traumatic syndromes, including stress, burnout, and emotional distress. Resilience and self-compassion may serve as protective factors in mitigating stress and burnout stemming from the pandemic. Moreover, these factors may contribute to posttraumatic growth (PTG), which has been recognized as a potential outcome for nurses caring for patients. This study aimed to investigate the factors contributing to PTG among registered nurses, with perceived stress, burnout, resilience, and self-compassion.
Methods
This cross-sectional observational survey used convenience sampling with 228 registered nurses from New York. Data were collected online using self-reported measures of the following study variables: perceived stress, burnout (sub-dimensions: emotional exhaustion, depersonalization, and personal accomplishment), resilience, self-compassion, and PTG. The data were analyzed using path analysis.
Results
Resilience and self-compassion directly and positively affected PTG, while perceived stress and burnout indirectly affected PTG via resilience and self-compassion. Among three sub-dimensions of burnout, PTG was indirectly affected by emotional exhaustion via resilience, depersonalization via self-compassion, and personal accomplishment via resilience and self-compassion.
Discussion
This study identifies resilience and self-compassion as key psychological resources that directly enhance nurses’ PTG, while perceived stress and burnout undermine it indirectly through these traits. Each burnout dimension had distinct mediating pathways: emotional exhaustion through resilience, depersonalization through self-compassion, and low personal accomplishment through both. These findings emphasize the need for targeted interventions that strengthen resilience and self-compassion while addressing specific burnout symptoms. Limitations include the cross-sectional, self-reported nature of the data and limited generalizability. Longitudinal studies are needed to confirm these pathways and inform intervention design.
Conclusion
The findings of this study suggest that resilience and self-compassion are essential in promoting PTG among nurses, helping them better cope with COVID-related stress and burnout. This study investigates the dynamic role of resilience alongside self-compassion, demonstrating how these factors interact with three distinct dimensions of burnout to influence PTG outcomes. Therefore, the study emphasizes the need for multifaceted interventions, such as mindfulness programs, resilience training, and self-compassion initiatives, to enhance nurses' resilience and self-compassion. These interventions effectively reduce stress and burnout while promoting PTG both during and beyond the COVID-19 pandemic.
1. INTRODUCTION
The Coronavirus 2019 (COVID-19) pandemic has significantly impacted healthcare professionals worldwide. Nurses especially have been greatly affected due to their constant care for suspected and confirmed cases under extremely challenging conditions: increased workloads, both in terms of patient numbers and working hours and exposure to the highest risk of infection [1-6]. These immense pressures have resulted in nurses experiencing high levels of stress and burnout, psychological distress, and posttraumatic stress symptoms [1, 4, 7-15]. Despite these extensively critical challenges, researchers have also been exploring the potential positive outcomes that might impact nurses' post-traumatic growth (PTG) [15-21].
In a study conducted by Chen and colleagues in 2021 involving 12,596 nurses during the pandemic, it was found that nurses encountered traumatic responses, including feelings of irritation, frequent anger, nervousness, sleep difficulties, unhappy thoughts, distressing memories, and emotional exhaustion, which were categorized as burnout. The trauma experienced by the nurses was attributed to the high-intensity workload and uncertainty associated with COVID-19. These traumatic responses were linked to acute stress reactions and persistent changes in the body's physiological, emotional, and cognitive responses [22].
In addition, Bruyneel et al.’s study revealed that out of 1,135 nurses surveyed, the prevalence of burnout risk was found to be 68% [2]. The burnout as a long-lasting negative consequence has been identified as having three dimensions: emotional exhaustion, depersonalization, and personal accomplishment [23, 24]. Notably, during the pandemic, emotional exhaustion has emerged as a leading contributing factor to burnout in nurses. This involves feelings of being drained, fatigued, frustrated, strained, and burned out from work [2, 25-27].
PTG is a phenomenon that refers to positive change that occurs as a result of struggling with highly challenging life circumstances [17]. The COVID-related highly stressful crises have the potential to function as a catalyst for PTG, which can serve as a coping resource that is linked to preventing and minimizing distressing experiences in nurses [15, 16, 18-21, 28]. Based on Chen et al.’s research findings, it was revealed that 39% of nurses underwent PTG. Additionally, a study by Cui et al., which involved 167 nurses, demonstrated that the participating nurses experienced varying degrees of PTG, ranging from moderate to high levels [16, 19].
Resilience and self-compassion are increasingly recognized as crucial protective factors in mitigating stress and burnout while fostering PTG. Resilience, defined as the ability to adapt positively to adversity, plays a critical role in buffering against stress and burnout, ultimately promoting PTG.
Previous research conducted with nurses has demonstrated a significant negative correlation between resilience and perceived stress [29, 30], as well as burnout (personal, work-related, and client-related) [25, 27, 30-33]. In addition, studies conducted by Atay et al. and Liu et al. reveal that resilience is positively associated with PTG among nurses caring for patients with COVID-19 [18, 21]. Moreover, research studies have indicated that resilience plays a significant role in mediating COVID-related stress and PTG in non-medical individuals [34, 35]. Similarly, resilience serves as a mediator between burnout and PTG among healthcare professionals [36]. These findings suggest that resilience may serve as a psychological mechanism through which stress and burnout influence PTG.
Similarly, self-compassion - characterized by self-kindness, mindfulness, and common humanity - has been identified as a psychological resource that helps individuals navigate distressing experiences. Research has demonstrated that self-compassion may buffer the negative impacts of stress and burnout on healthcare providers, including nurses [7, 37-42], and may protect and empower nurses to cope with distress [43]. In addition, research has shown that self-compassion is positively linked to PTG in the face of trauma [7, 44, 45]. As a result, self-compassion has the potential to act as a safeguard against emotional exhaustion and distress among nurses and can also facilitate positive growth, particularly in the aftermath of traumatic events [46-48].
Despite growing evidence supporting the benefits of resilience and self-compassion, to the best of our knowledge, no study has investigated the effects of resilience and self-compassion predictor of stress, burnout, and PTG among nurses during the COVID-19 pandemic. In addition, no studies have explored the distinct effects of each dimension of burnout on PTG.
By identifying the impact of resilience and self-compassion on PTG, including the impacts of each dimension of burnout, this study can enhance our comprehension of PTG. This can enable the development of affordable interventions that aim to reduce stress and burnout while using resilience and self-compassion as coping strategies. Ultimately, these interventions could empower nurses to experience positive personal growth even in the face of traumatic situations.
This study aims to investigate the factors contributing to PTG, including perceived stress, burnout, resilience, and self-compassion. Our hypotheses are as follows: (1) resilience and self-compassion have a direct effect on PTG; (2) perceived stress and burnout indirectly affect PTG via resilience and self-compassion.
2. METHODS
2.2. Sample and Settings
This study involved 228 nurses recruited via convenience sampling from hospitals and healthcare facilities in the community, including long-term care centers and nursing homes in New York. The inclusion criteria for participation were as follows: (1) participants were aged 18 years or older, (2) employed full-time (a minimum of 35 hours per week) as registered nurses, (3) directly involved in providing healthcare services to patients infected with COVID-19 during the pandemic, and (4) provided voluntary informed consent to participate. The exclusion criteria included individuals who were not employed full-time as registered nurses or who did not have direct involvement in providing healthcare services to patients infected with COVID-19 during the pandemic.
The sample size was determined based on the recommendation that at least 200 responses would be necessary for conducting valid structural equation modeling research [49]. Therefore, the researchers screened the eligible nurses and selected 250 participants who met the inclusion criteria. However, 22 participants with incomplete answers were excluded, which led to 228 participants being included in the final analysis.
2.3. Data Collection
This study was approved by the institutional review board at the first author's college (approval number: 2021-0117) and was funded by the Professional Staff Congress-City University of New York Grant (No. 65189-00 53). After approval was obtained from the nursing department directors of three hospitals and the presidents of two regional nursing organizations, flyers were distributed for recruitment. In addition, we posted the study flyers on the websites of other nursing organizations, and working nurses who expressed interest accessed an individual Survey Monkey™ link, where they received an informed consent form with information about the study's purpose, the participant's rights to confidentiality, voluntary participation, withdrawal, and the study's risks and benefits. Those who provided informed consent were enrolled, completed the study questionnaire, and provided information regarding their demographics. All participants received a $10 Amazon card for completing the questionnaires. The survey took approximately 15-20 minutes to complete. We utilized validated tools in data collection to minimize bias. Data was collected from July through September 2022 in New York.
2.4. Measures
Each measure was chosen due to its proven reliability, validity, and relevance to the study's objectives.
2.4.1. Perceived Stress
Perceived stress was assessed using the 10-item Perceived Stress Scale (PSS) [50]. Each item is rated on a 5-point Likert scale (0: Never - 4: Very Often), with higher scores indicating higher levels of perceived stress. The PSS has demonstrated good reliability (α = .84) [50]. In this study, Cronbach's α was 0.87.
2.4.2. Burnout
Burnout was assessed using the Maslach Burnout Inventory Human Services Survey for Medical Personnel [MBI-HSS (M.P.)] [23, 24]. The MBI-HSS (M.P.) consists of 22 items that assess three dimensions of burnout in medical personnel: Emotional Exhaustion (9 items), Depersonalization (5 items), and Personal Accomplishment (8 items). Each item is rated on a 7-point Likert scale (0: Never - 6: Every Day), with higher scores indicating higher levels of burnout. Participants with scores of 0–18, 19–26, and ≥ 27 on the emotional exhaustion scale exhibit low, moderate, and high levels of emotional exhaustion, respectively. Those scoring 0–5, 6–9, and > 9 in the depersonalization dimension have low, moderate, and high levels of depersonalization, respectively. Items in the dimension measuring poor personal accomplishment are reverse coded; participants with scores of 0–33, 34–39, and ≥ 40 exhibit a low, moderate, and high degree of poor personal accomplishment, respectively. In this study, Cronbach's α was 0.92 for emotional exhaustion, 0.8 for depersonalization, and 0.80 for personal accomplishment.
2.4.3. Resilience
Resilience was assessed using the 25-item Connor-Davidson Resilience Scale (CD-RISC) [51]. Each item is rated on a 5-point Likert scale (0: Not true at all - 4: True nearly all of the time). Total scores range from 0 to 100, with higher scores indicating greater resilience. Studies have supported high internal consistency and test-test reliability [52]. Cronbach's α was 0.89 in the original Connor-Davidson resilience scale and 0.95 in this study [51].
2.4.4. Self-compassion
Self-compassion was assessed using the 12-item Self-Compassion Scale Short-Form (SCS-SF) [53]. Each item is rated on a 5-point Likert scale (1: Almost Never - 5: Almost Always). The SCS-SF has demonstrated excellent internal consistency (α ≥ .86 in all samples) [53]. In this study, Cronbach's α was 0.82.
2.4.5. Posttraumatic Growth
PTG was assessed using the 10-item short form of the Posttraumatic Growth Inventory (PTGI-SF) [54]. Each item is rated on a 6-point Likert scale (0: I did not experience this change as a result of my crisis - 5: I experienced this change to a very great degree as a result of my crisis). Total scores range from 0 to 60, with higher scores indicating greater levels of PTG. Cronbach's α was 0.90 in the original study of the short-form and 0.90 in this study [54].
2.5. Data Analysis
The data were analyzed using SPSS version 26.0 and AMOS version 26.0 (IBM Corp., Armonk, NY, USA). Path analysis was utilized in this study as a straightforward method for testing the proposed relationships without requiring a latent construct. Descriptive statistics and Pearson correlation coefficients were used to summarize each of the study variable scores and to explore correlations between variables, respectively. We analyzed variables as continuous data without grouping. The variables' normality was examined with skewness and kurtosis. Model fit was analyzed using the following indices: chi-square mean/degree of freedom (CMIN/DF, χ2/df), comparative fit index (CFI), and Tucker Lewis index (TLI, values > .90 represent an acceptable fit and >.95 a good fit), standardized root mean square residual (SRMR, <0.08 indicated acceptable fit), and root mean square error of approximation (RMSEA, ≤0.06 with a CI of 0.00–0.08 indicated a good fit) [50]. Indirect effects were tested using the bootstrapping approach considering a 95% confidence interval (CI; bootstrap replications: 1,000).
3. RESULTS
3.1. Participants' Characteristics
A total of 228 nurses participated in this study. Participants' mean age was 41.95 years (standard deviation [S.D.] = 12.21, range 22 –71). More than four-fifths (83.3%) were female; Asian were 62.7%, followed by White (14.0%), Hispanic/Latino (7.9%), and African American (6.1%). More than 89% held a bachelor's degree or higher. Most (78.1%) were registered nurses (RN), followed by nurse practitioners (12.7%), and nurse managers. On average, participants had worked as an RN for 158.37 months (SD = 136.02), with 46.8% working for more than 10 years. Most (82.9%) worked in hospitals. In addition, 87.6% had taken care of COVID-19 patients since March 2020.
3.2. Descriptive Statistics and Correlations
Descriptive statistics and correlations of study variables are presented in Table 1.
PTG was significantly positively correlated with resilience (r = .60, p < .001), self-compassion (r = .43, p < .001), and personal accomplishment (r = .39, p < .001). PTG was negatively correlated with stress (r = -.35, p < .001), depersonalization (r = -.26, p < .001) and emotional exhaustion (r = -.28, p < .001).
3.3. Testing the Hypothetical Model
The results of the path analysis revealed an acceptable fit to the observed data (CMIN/DF = 3.783, CFI = .980, TLI = .914, RMSEA = .111, and SRMR = .0343). However, the two paths were nonsignificant. To enhance clarity, the model was modified by removing the nonsignificant paths (from Depersonalization to resilience and emotional exhaustion to self-compassion). The statistical justification was based on the modification indices and standardized path coefficients. Overall, the fit indices demonstrated a good fit between the data and the modified model: χ2(df) = 19.012 (7), p < .05, CMIN/DF = 2.716, CFI = .982, TLI = .947, RMSEA = .087, and SRMR = .0347.
The results of the path analysis (Table 2) indicated that resilience and self-compassion directly affect PTG (β = .52, p = .004; β = .15, p = .025, respectively). Stress, personal accomplishment, and emotional exhaustion directly affect resilience (β = -.35, p = .003; β = .28, p = .002; β = -.25, p = .002, respectively). Stress, depersonalization, and personal accomplishment directly affect self-compassion (β = -.53, p = .003; β = -.14, p = .016; β = .13, p = .008, respectively). Stress [β = -.26, .95% CI (-.366, -.163)] and all three burnout factors—depersonalization [β = -.02, 95% CI (-.058, -.003)], personal accomplishment [β = .17, 95% CI (.081, .252)], and emotional exhaustion [β = -.13, 95% CI (-.217, -.061)]—indirectly influence PTG (Table 2 & Fig. 1).
| Variables | r (p) | Mean ± SD | |||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5a | 5b | - | |
| 1. Posttraumatic Growth |
1 | - | - | - | - | - | 33.95 ± 9.07 |
| 2. Resilience | .60 (.00) |
1 | - | - | - | - | 68.32 ± 14.85 |
| 3. Self-Compassion | .43 (.00) |
.56 (.00) |
1 | - | - | - | 38.31 ± 7.58 |
| 4. Stress | -.35 (.00) |
-.61 (.00) |
-.65 (.00) |
1 | - | - | 18.52 ± 6.14 |
| 5a. Burnout (DP) | -.26 (.00) |
-.44 (.00) |
-.47 (.00) |
.53 (.00) |
1 | - | 9.70 ± 7.12 |
| 5b. Burnout (PA) | .39 (.00) |
.46 (.00) |
.38 (.00) |
-.39 (.00) |
-.33 (.00) |
1 | 34.38 ± 7.66 |
| 5c. Burnout (EE) | -.28 (.00) |
-.50 (.00) |
-.44 (.00) |
.61 (.00) |
.66 (.00) |
-.16 (.014) |
28.51 ± 12.93 |
| Endogenous Variables | Exogenous Variables | SMC | Direct β |
Indirect β |
Total β |
|---|---|---|---|---|---|
| Posttraumatic Growth | Resilience | .36 | .52** | - | .52** |
| Self-Compassion | - | .15* | - | .15* | |
| Stress | - | - | -.26** | -.26** | |
| Burnout (EE) | - | - | -.13*** | -.13*** | |
| Burnout (DP) | - | - | -.02* | -.02* | |
| Burnout (PA) | - | - | .17** | .17** | |
| Resilience | Stress | .47 | -.35** | - | -.35** |
| Burnout (EE) | - | -.25** | - | -.25** | |
| Burnout (DP) | - | - | - | - | |
| Burnout (PA) | - | .28** | - | .28** | |
| Self- Compassion |
Stress | .46 | -.53** | - | -.53** |
| Burnout (EE) | - | - | - | - | |
| Burnout (DP) | - | -.14* | - | -.14* | |
| Burnout (PA) | - | .13** | - | .13** |
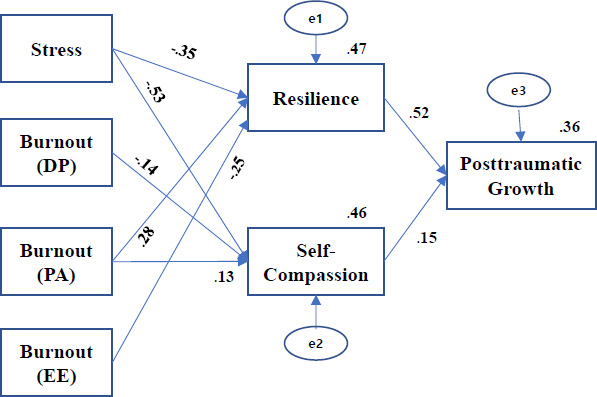
Path model of posttraumatic growth with standardized path coefficients (β). Note: DP = Depersonalized; PA = Personal Accomplishment; EE = Emotional Exhaustion.
Table 2 also shows the total, direct, and indirect effects of the study variables on PTG. Overall, the modified model explained 47.0% of the variance in resilience and 36.0% of the variance in PTG. A final path model with the standardized coefficients and the square root (R2) is presented in Fig. (1).
4. DISCUSSION
This study identified the factors contributing to PTG among nurses during the COVID-19 pandemic. Findings indicate that resilience and self-compassion directly positively affected PTG, while perceived stress and burnout indirectly negatively affected it. These results are consistent with previous research that found a positive association between resilience and PTG [18, 21] and between self-compassion and PTG in nurses [7, 44]. For instance, studies found that resilience was positively associated with PTG in nurses working at pandemic clinics and caring for COVID-19 patients [18, 21]. Additionally, a study of Korean nurses working in intensive care units found that self-compassion predicted PTG [44]. This is likely because resilience and self-compassion are linked to the use of adaptive coping strategies after experiencing trauma, which can facilitate PTG [7, 18, 20, 21, 31, 34, 44, 45, 55]. Together, these findings suggest that strengthening psychological resilience and positive self-compassion may have beneficial effects on improving PTG in nurses.
The findings of our study indicate that the perception of stress and burnout can have a negative effect on resilience and self-compassion. These findings align with previous research that suggests that resilience can mitigate the negative consequences of stress and burnout among nurses during the COVID-19 pandemic [12, 25, 27, 29, 31, 33, 36]. In addition, previous studies have demonstrated that self-compassion is inversely linked to perceived stress and burnout among nurses and healthcare providers [38, 39, 41, 56], which is consistent with our findings. Interventions focusing on self-compassion have proven effective in reducing stress and burnout among nurses. For instance, after a day of self-compassion training during the COVID-19 pandemic, nurses reported a significant improvement in self-compassion and a decrease in perceived stress, burnout, and anxiety [46]. Another study found that a 4-hour mindfulness workshop successfully reduced nurses' perceived stress and burnout, with a positive effect sustained even at 6-month post-tests [57]. Our study, in combination with the above findings, emphasizes the importance of preventing and minimizing perceived stress and burnout for promoting PTG.
A study with 375 nurses in Spain who cared for COVID-19 patients found that all three dimensions of burnout (emotional exhaustion, depersonalization, and personal accomplishment) were inversely related to resilience [32]. Similarly, a study with healthcare professionals found that self-compassion was negatively associated with burnout [41]. In contrast, our study demonstrated that resilience was differentially influenced by the impact of each dimension of burnout when self-compassion was also considered. Emotional exhaustion indirectly affected PTG via resilience but not self-compassion, while depersonalization was mediated by self-compassion alone. Resilience helps individuals deal with stress and emotional energy and, therefore, may be closely linked to the emotional exhaustion dimension of burnout [58]. In contrast, symptoms of depersonalization, such as unfeeling and impersonal responses toward patients, appear to be more relevant to self-compassion that involves emotional warmth and empathy. Low personal accomplishment indirectly influenced PTG via resilience but also had a significant indirect effect on PTG via self-compassion. This is in line with previous findings that beliefs about one’s competence in attaining desired achievement are positively correlated with resilience in times of stress by promoting a sense of control [59]. In addition, the unconditional self-acceptance and supportive nature of self-compassion contribute to PTG as on deals with difficult experiences [47]. Although further research is needed to confirm our findings, our study suggests that examining the level of each dimension of burnout separately from the others may offer a more comprehensive understanding of predicting PTG and enable tailored interventions based on individual needs rather than solely relying on the total burnout scores.
The study's clinical implications underscore the need for healthcare organizations to assess nurses' stress and burnout levels periodically, creating a healthy work environment that incorporates organizational support and training opportunities. These provisions enable nurses to enhance their ability to cope with challenging situations. Programs aimed at fostering PTG should primarily focus on building resilience and self-compassion. Practical strategies include conducting informative sessions on self-care, organizing interprofessional workshops with psychological professionals to enhance resilience, and establishing a network of professionals accessible to nursing staff. Additionally, implementing interventions such as mindfulness activities, self-compassion workshops, peer support groups to foster connection and empathy, and the creation of dedicated “relaxation rooms” can cultivate a sense of self-acceptance among nurses. Partnering with local nursing associations to streamline institutional support and implement interventions focused on resilience and self-compassion is also vital. Moreover, these findings suggest incorporating these elements into nursing education curricula to better prepare future nurses.
To promote PTG in nurses by enhancing resilience, we also suggest the importance of organizational support. Studies have reported the beneficial effects of organizational support on nurses [18, 60]. For instance, one study found a positive correlation between perceived organizational support and psychological resilience among Turkish nurses working in pandemic clinics [60]. Furthermore, another study of nurses working at pandemic clinics in Turkey reported that nurses who perceived that they had organizational support from nursing service management had higher levels of resilience and PTG [24]. These findings highlight the beneficial influence of organizational support in fostering PTG by strengthening resilience. Therefore, we suggest that interventions that enhance resilience should include ongoing psychological and organizational support, comprehensive training and communication, and the provision of a healthy workplace environment [11, 14, 19, 36, 45-47, 61]. It is also essential to ensure that nurses have access to support, protection, and counseling to protect their mental well-being and prevent adverse consequences, such as stress and burnout. Providing comprehensive interventions that enhance nurses' resilience can promote positive transformations and potential outcomes such as PTG.
Our study's findings present a comprehensive overview of both direct and indirect factors contributing to PTG, which is noteworthy considering that previous studies did not explore the relationships among the variables included in this study. However, further research is necessary to investigate the interrelationships between antecedents and outcomes of PTG that were not examined in our study. Moreover, some studies have found that factors based on the PTG theory [16], such as deliberate rumination, can influence PTG among nurses in China and Korea [19, 28]. Therefore, examining other factors that impact PTG in addition to the variables analyzed in this study would be beneficial, as that can enhance our understanding of the phenomenon. Further investigating the factors influencing PTG can help to build support for nurses who face significant stress and burnout during pandemics like COVID-19. Moreover, the findings of this study can be generalized to the post-COVID-19 period by recognizing that the psychological challenges nurses faced during the pandemic are not exclusive to that context. Stress, burnout, and exposure to traumatic situations are inherent to nursing, especially in high-pressure environments such as critical care, emergency departments, and disaster response scenarios.
The attributes, resilience and self-compassion, are not pandemic-specific but are essential for coping with any form of workplace adversity or trauma. Interventions aimed at enhancing resilience and fostering self-compassion, such as mindfulness training and peer support programs, can be valuable for nurses in various clinical settings, whether during routine operations or crises. The negative impact of stress and burnout on PTG underscores the need for ongoing strategies to monitor and mitigate these issues, regardless of the pandemic. Healthcare organizations can implement regular well-being assessments, provide psychological support services, and design stress-reduction initiatives as part of standard practice, helping nurses maintain optimal mental health and professional performance.
Additionally, the study's findings on coping mechanisms and organizational support can be extended to other public health crises or natural disasters, where nurses play a critical role in responding to emergencies. This adaptability suggests that fostering resilience and self-compassion should be integral components of preparedness plans for future crises. By applying these findings beyond the pandemic, healthcare systems can better support nurses' psychological well-being, enhance their capacity for PTG, and build a resilient workforce capable of thriving in the face of ongoing challenges.
5. LIMITATIONS
While this study provides important insights into the relationships between perceived stress, burnout, resilience, self-compassion, and PTG among nurses during the COVID-19 pandemic, some limitations should be considered. First, the study indirectly assessed traumatic experiences by measuring perceived stress and burnout levels during the pandemic. Future research could explore how different types and degrees of trauma exposure may impact the study results. Second, the study employed a cross-sectional design, which means that causal relationships among the variables of interest could not be evaluated. Future studies using a longitudinal design would provide a better understanding of the interrelationships between variables over time and identify causal implications. Third, the reliance on self-reported data represents the possibility of response bias, as participants' perceptions and recollections may be influenced by personal experiences or social desirability. Fourth, collecting data through an online survey could have introduced selection bias as it only included individuals with internet access. However, the participants in this study were college students who typically have reliable internet access. Although significant, the finding of indirect path coefficients was small. However, small indirect effects can still have practical significance. Future research with larger sample sizes may help clarify the stability and strength of these effects. Finally, the use of convenience sampling may restrict the generalizability of the findings. It is recommended that future studies employ random sampling methods to enhance validity. Additionally, to further improve the generalizability, replicating the findings in more diverse populations and settings across various global regions would be valuable. By doing so, we can understand how different contexts may influence the relationships between the variables of interest.
CONCLUSION
This study explored factors contributing to PTG in nurses, including perceived stress, burnout, resilience, and self-compassion. The findings revealed that PTG is directly influenced by resilience and self-compassion and indirectly by perceived stress and burnout. This study examines how the three sub-dimensions of burnout interact with resilience and self-compassion to influence PTG. Resilience enables individuals to manage the emotional exhaustion dimension of burnout, while self-compassion is more closely associated with the depersonalization dimension, as it fosters emotional warmth and empathy. The low personal accomplishment dimension influences PTG through both resilience and self-compassion, consistent with research linking perceived competence to resilience under stress. Furthermore, the supportive nature of self-compassion contributes to PTG during adversity. These findings recommend that analyzing the dimensions of burnout separately may offer a more comprehensive approach to predicting PTG and developing targeted interventions rather than relying solely on a single domain of burnout. Consequently, this study suggests implementing multifaceted interventions, such as mindfulness programs, resilience training, and self-compassion interventions, to strengthen nurses' resilience and self-compassion. These approaches can effectively mitigate stress and burnout while fostering PTG during the COVID-19 pandemic.
AUTHORS’ CONTRIBUTIONS
The authors confirm contribution to the paper as follows: Conceptualization, S.H. and H.S.K.; methodology, S.H., H.S.K., K.E., K.K., and F.A.; software, S.H. and H.S.K.; validation, S.H., H.S.K., K.E., K.K., and F.A.; formal analysis, H.S.K. and S.H.; investigation, S.H., K.K., and F.A.; resources, S.H., K.K., and F.A.; data curation, H.S.K. and S.H.; writing—original draft preparation, S.H., H.S.K., K.E., K.K., and F.A.; writing—review and editing, S.H., H.S.K., K.E., K.K., and F.A.; visualization, S.H. and H.S.K.; supervision, S.H.; project administration, S.H. All authors have read and agreed to the published version of the manuscript.
LIST OF ABBREVIATIONS
| PTG | = Posttraumatic Growth |
| COVID-19 | = Coronavirus 2019 |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval was obtained from the institutional review board of the LaGuardia Community College (approval number 2021-0117).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data supporting this study are available from the corresponding author [K.E] upon reasonable request.
FUNDING
This research was funded by Professional Staff Congress-City University of New York (No. 65189-00 53) funding.
ACKNOWLEDGEMENTS
We acknowledge the support of the Professional Staff Congress-City University of New York (PSC-CUNY) under Grant No. 65189-00 53.