All published articles of this journal are available on ScienceDirect.
Nurses’ Knowledge of Diabetic Foot Ulcer Management in North Vietnam
Abstract
Background
Diabetic Foot Ulcers (DFUs) are a serious complication of diabetes. Nurses play a critical role in DFU management; however, their knowledge remains inconsistent. Therefore, assessing nurses’ knowledge of DFU management is essential to identify knowledge gaps and utilize them to improve the quality of care.
Objective
This study aimed to assess nurses' knowledge in managing DFUs in the northern provinces of Vietnam.
Methods
A cross-sectional study was conducted across 12 northern provinces of Vietnam from August 2023 to April 2024. A questionnaire focusing on DFU management was developed to assess the knowledge of 560 nurses from 18 provincial and 22 district hospitals. Nurses’ knowledge was evaluated based on the percentage of correct answers to each question: more than 50% (Level 1); and 50% or less (Level 2).
Results and Discussion
The majority of nurses demonstrated Level 2 knowledge, with 24.3% answering all 7 questions at this level, while only 0.4% answered all questions at Level 1. Over 80% of nurses had inadequate knowledge of DFU management. Nurses who had participated in wound care training scored significantly higher at Level 1, compared to those without training (29.5 ± 7.6 vs. 14.3 ± 6.4, p < 0.001). Knowledge levels did not differ significantly between nurses working at provincial and district hospitals (p > 0.05) nor between those with and without wound care experience (p > 0.05).
Conclusion
Nurses in northern Vietnam demonstrated limited knowledge in managing DFUs. Workplace and wound care experience were not significantly associated with knowledge levels. However, wound care training was significantly associated with higher knowledge levels. These findings underscore the importance of implementing structured wound care training programs for nurses. Future research should explore the effectiveness of various training approaches in improving clinical outcomes for patients with DFUs.
1. INTRODUCTION
Diabetic Foot Ulcers (DFUs) are a common complication in patients with diabetes. Each year, approximately 18.6 million people suffer from DFUs worldwide [1]. The burden of DFUs is substantial, and Vietnam is no exception to this issue [2]. In Vietnam, diabetes is projected to become one of the top seven diseases causing death and disability by 2030 [3, 4]. Many studies conducted in Vietnam have shown that 40% to 73% of patients are unaware that they have diabetes mellitus [5, 6]. As a result, many diabetic patients who seek medical care already present with complications.
DFUs often result from complications such as peripheral arterial disease, neuropathy, and poor wound healing conditions that are routinely handled in the Trauma and Orthopedics, Cardiology, Endocrinology, and Neurology departments. Nurses in these settings are directly involved in wound care, monitoring of diabetic complications, and patient education, making their knowledge essential to effective DFU management and improved outcomes.
The care and treatment of patients with DFUs heavily depend on the knowledge and skills of healthcare providers, particularly nurses, at the primary healthcare level. Several studies have indicated that patients’ lack of awareness regarding diabetic foot care is closely linked to insufficient nursing support [7-10]. However, research on nurses' knowledge in this area in Vietnam remains limited.
The current situation in Vietnam is that DFU patients with multiple complications, difficult-to-treat wounds, and a high risk of limb amputation are often not managed at the primary healthcare level. Instead, most of these patients are referred to central healthcare facilities affiliated with the Ministry of Health. This study aimed to assess the level of knowledge among nurses working in primary healthcare facilities in Northern Vietnam regarding the management of DFUs. Specifically, the research sought to (1) evaluate nurses’ knowledge across different clinical domains of DFU management and (2) examine the associations between nurses’ knowledge levels and factors such as workplace setting, wound care experience, and prior wound care training.
2. METHODS
We conducted a cross-sectional survey from August 2023 to April 2024 in four target departments, namely Trauma and Orthopedics, Cardiology, Endocrinology, and Neurology, across 18 provincial hospitals and 22 district hospitals located in 12 provinces in Northern Vietnam.
2.1. Sampling Methods
A purposive sampling method was employed to select participants. This approach was chosen because it allows for the inclusion of nurses with relevant experience and knowledge in managing DFUs. All eligible nurses were invited to participate in the survey.
2.2. Inclusion Criteria
The study included nurses working in the selected departments (Trauma and Orthopedics, Cardiology, Endocrinology, and Neurology) of the 18 provincial hospitals and 22 district hospitals in 12 provinces in Northern Vietnam. Eligible participants were those who met the following inclusion criteria:
1. Nurses who had worked in the selected departments for at least six months at the time of the survey.
2. Nurses who were available during the study period (August 2023 to April 2024).
3. Nurses who were directly involved in patient care, including wound care, monitoring diabetic complications, and patient education.
2.3. Exclusion Criteria
Nurses were excluded from participation in the study if they met any of the following conditions:
1. Nurses who were assigned exclusively to administrative, managerial, or research roles and thus were not directly engaged in clinical patient care, including wound care, monitoring diabetic complications, and patient education.
2. Nurses with less than six months of continuous experience in the targeted departments at the time of data collection.
3. Nurses who declined to participate in the study or withdrew their informed consent at any stage of the survey process.
4. Nurses who had previously participated in similar studies on diabetic foot ulcer management within the past 12 months were excluded to minimize information bias.
2.4. Subjects
The study population consisted of 560 nurses. Among them, 265 nurses were working at provincial hospitals, and 295 nurses were working at district hospitals. Their average age was 34.8 ± 15.1 years (range: 23-50 years). Most nurses in this survey were female, accounting for 65%, while 35% were male. A total of 252 nurses (45%) had more than 5 years of wound care experience since graduating from nursing school (provincial hospital: 138 nurses [52.1%]; district hospital: 114 nurses [38.6%]). Additionally, 144 nurses (25.7%) had received wound care training after graduation (provincial hospitals: 95 nurses [35.8%]; district hospitals: 49 nurses [16.6%]). Most of the nurses participating in this survey (217 nurses [38.7%]) were working in the Endocrinology Department (provincial hospitals: 112 nurses [42.3%]; district hospitals: 105 nurses [35.6%]). Meanwhile, 172 nurses (30.7%) were working in the Trauma and Orthopedics Department, 106 nurses (18.9%) in the Cardiology Department, and 75 nurses (13.4%) in the Neurology Department (Table 1).
2.5. Questionnaire Form
The data were collected using a questionnaire developed by the researchers. The questionnaire consisted of two main sections. The first section included six items related to the socio-demographic and work-related characteristics of the participants, including age, gender, years of work experience, wound care experience, educational background, and current workplace. The second section comprised seven questions aimed at assessing nurses’ knowledge of DFU management. These questions were developed based on the guidelines provided by the American Diabetes Association (ADA) [11]. The contents of the questionnaire included the following components:
| Characteristics | Sub-groups | Provincial Hospital | District Hospital | Total | |||
|---|---|---|---|---|---|---|---|
| N (265) |
% | N (295) |
% | N (560) |
% | ||
| Age | Mean±SD | 35,5±12,7 | 32,8±13,7 | 34,8±15,1 | |||
| Min-max | 24-50 | 23-49 | 23-50 | ||||
| Gender | Male | 96 | 36.2 | 100 | 33.9 | 196 | 35 |
| Female | 169 | 63.8 | 195 | 66.1 | 364 | 65 | |
| Wound care experience* | < 5 years | 127 | 47.9 | 181 | 61.3 | 308 | 55 |
| ≥ 5 years | 138 | 52.1 | 114 | 38.6 | 252 | 45 | |
| Wound care training** | Yes | 95 | 35.8 | 49 | 16.6 | 144 | 25.7 |
| No | 179 | 64.1 | 146 | 83.4 | 416 | 74.3 | |
| Hospital Unit | Trauma-Orthopedics Dept | 71 | 26.8 | 101 | 34.2 | 172 | 30.7 |
| Cardiology Dept | 49 | 18.5 | 57 | 19.3 | 106 | 18.9 | |
| Endocrinology Dept | 112 | 42.3 | 105 | 35.6 | 217 | 38.7 | |
| Neurology Dept | 43 | 12.5 | 32 | 10.8 | 75 | 13.4 | |
** Nurses who have attended formal training courses after graduation.
- Question 1 (Q1 - Which of the following is a risk factor for diabetic foot ulcers?):
The risk factors for foot ulcers included eight options: previous amputation, history of foot ulcers, peripheral neuropathy, foot deformity, peripheral vascular disease, visual impairment, diabetic nephropathy (especially in patients on dialysis), and poor glycemic control.
- Question 2 (Q2 - Which of the following is/are part of the medical history relevant to diabetic foot ulcers?):
Medical history factors included six response options: ulceration, amputation, charcot joint, vascular surgery, angioplasty, and cigarette smoking.
- Question 3 (Q3-Which of the following is/are the symptom(s) of neuropathy in a patient with diabetic foot ulcers?): Symptoms of neuropathy had four response options: burning or shooting pain, electrical or sharp sensations, numbness, and lifeless feet.
-Question 4 (Q4 - Which of the following are cutaneous manifestations of diabetic foot ulcers?):
The options for foot skin manifestations included: soft skin, discoloration, thickening, dryness, cracking, excessive sweating, fungal infection between the toes, ulceration, calluses or blistering, and hemorrhage within calluses.
- Question 5 (Q5 - Which of the following procedure(s) is/are used to assess vascular status in diabetic ulcer?): Procedure(s) used to assess vascular status included four response options: Palpation of tibial and dorsalis pedis pulse, ABI, if indicated, Vascular ultrasound, Determination of SpO2.
- Question 6 (Q6 - Which of the following test(s) are commonly used to assess peripheral neuropathy in diabetic foot ulcers?):
The commonly used tests to assess peripheral neuropathy included: Semmes-Weinstein monofilament test, 128-Hz tuning fork, pinprick sensation, and ankle reflexes.
- Question 7 (Q7 - What are the preventive measures for managing diabetic foot ulcers?):
This question aimed to assess nurses’ knowledge of preventive management and included six response options: daily foot inspection, proper footwear, blood sugar control, weight loss, foot skin and toenail care, and protective surgeries.
2.6. Data Collection Methods
This survey was approved by the hospital leadership at each participating site. Data were collected by trained health professionals who were instructed in standardized procedures before the implementation of the survey. Eligible nurses were provided with detailed information regarding the study’s objectives and procedures. Written informed consent was obtained from all participants before their enrollment in the study, and participation was entirely voluntary.
All eligible nurses working in the selected departments during the study period were invited to complete the questionnaire. Participants were instructed to read each question carefully and select only the responses they believed to be correct, leaving any items blank if they were unsure or believed the options were incorrect. Each nurse was allotted 15 minutes to complete the questionnaire, which consisted of 13 items as previously described. All invited participants completed and returned the questionnaire.
2.7. Evaluation Methods
The classification of knowledge levels was based on the percentage of correct responses, which was considered indicative of the participants’ overall knowledge. Two levels were defined: Level 1 included nurses who selected more than 50% of the correct options in a given question, while Level 2 included those who selected 50% or fewer of the correct options. This approach allowed for a more nuanced assessment of partial knowledge, especially for questions with multiple correct answers.A 50% threshold was chosen as a straightforward and practical criterion for classifying knowledge levels. This cut-off point provided a clear distinction between participants with relatively higher and lower levels of knowledge. It has also been widely used in previous studies evaluating healthcare workers' knowledge in similar contexts [12, 13].
2.8. Statistical Analysis
The survey data were recorded, coded, and analyzed using Stata 11.0 software. The percentage of correct responses was used as an indicator of the participants' overall knowledge level. To compare the mean values and distributions between groups, the T-test and Chi-Square tests were applied. A p-value of ≤ 0.05 was considered statistically significant.
3. RESULTS
The overall findings are presented in Table 2. At Level 1, the majority of nurses correctly answered only one question, which accounted for the highest percentage at 28.4%. This proportion gradually decreased, with 15.4% of nurses answering two questions correctly and only 0.4% answering all seven correctly. In contrast, at Level 2, the number of nurses answering more questions incorrectly increased. The range varied from 12.5% answering one question incorrectly to 24.3% answering all seven questions incorrectly at this level.
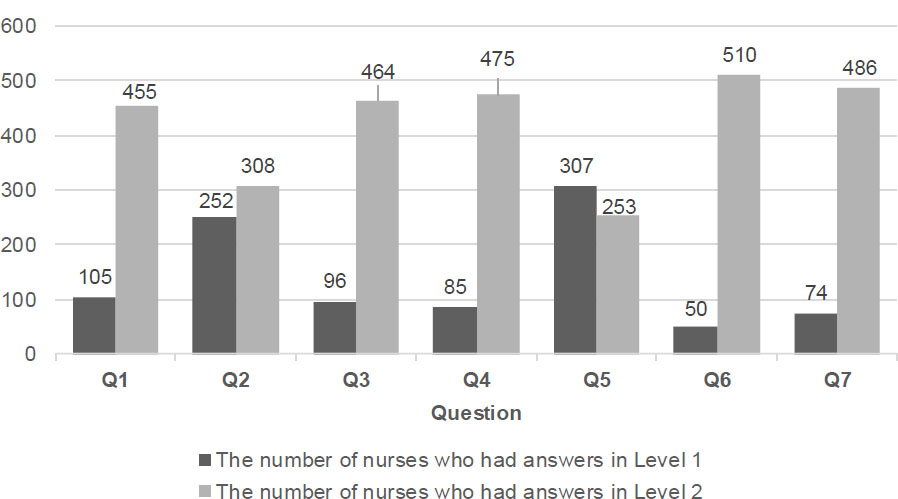
A notably high proportion of nurses were at Level 2. Specifically, 308 nurses (55%) were at Level 2 for Question 2 (Medical history of DFU), and 253 nurses (45.2%) for Question 5 (Procedures used to assess vascular status in diabetic ulcers). For the remaining questions (Q1, Q3, Q4, Q6, and Q7), over 80% of the nurses were at Level 2. Notably, for Question 6 (Tests commonly used to assess peripheral neuropathy in DFUs), 510 nurses (91.1%) were at Level 2. In contrast, the proportion of nurses at Level 1 was very low (Fig. 1).
| Number of Questions | The Number of Nurses who had Answers In | |||
|---|---|---|---|---|
| Level 1 | Level 2 | |||
| N | % | N | % | |
| 1 | 159 | 28.4 | 70 | 12.5 |
| 2 | 86 | 15.4 | 71 | 12.7 |
| 3 | 75 | 13.4 | 74 | 13.2 |
| 4 | 57 | 10.2 | 85 | 15.2 |
| 5 | 27 | 4.8 | 101 | 18.0 |
| 6 | 6 | 1.1 | 120 | 21.4 |
| 7 | 2 | 0.4 | 136 | 24.3 |
Nurses’ knowledge levels on DFU management by survey question (n=560).
| Criteria | Subgroup | Level 1 | Level 2 | ||
|---|---|---|---|---|---|
|
Mean* ± SD (95% CI) |
p-value |
Mean* ± SD (95% CI) |
p-value | ||
| Workplace | Provincial hospital (n=265) |
25.4 ± 6.2 (16.2-30.5) |
0.23 | 53.4 ± 12.6 (35.4-60.3) |
0.45 |
| District hospital (n=295) |
23.2 ± 7.1 (13.3-29.8) |
56.4 ± 13.2 (36.6-63.7) |
|||
| Wound care experience | < 5 years (n=308) |
18.6 ± 5.6 (13.9-22.4) |
0.17 | 59.2 ± 14.2 (39.5-65.3) |
0.52 |
| ≥ 5 years (n=252) |
20.6 ± 6.0 (15.9-24.8) |
57.7 ± 15.3 (37.4-68.8) |
|||
| Wound care training | Yes (n=144) |
29.5 ± 7.6 (18.9-30.7) |
≤ 0.001 | 32.6 ± 15.2 (24.5-35.5) |
≤ 0.001 |
| No (n=416) |
14.3 ± 6.4 (8.2-18.3) |
58.3 ± 13.6 (38.8-67.2) |
|||
*Percentage of correct answers.
The relationship between response levels and the proposed criteria is shown in Table 3. Nurses who had attended wound care training courses demonstrated significantly higher Level 1 knowledge (29.5 ± 7.6 vs. 14.3 ± 6.4; p < 0.001)and significantly lower Level 2 knowledge (32.6 ± 15.2 vs. 58.3 ± 13.6; p < 0.01), compared to those who had not attended the training. There were no statistically significant differences in knowledge levels between nurses working in provincial versus district hospitals (p > 0.05). Additionally, wound care experience was not significantly related to knowledge levels among nurses (p > 0.05) (Table 3).
4. DISCUSSION
4.1. Nurses’ Knowledge of DFU Management
Hospital overcrowding remains a significant challenge in Vietnam, placing considerable strain on healthcare facilities. Efforts to strengthen primary healthcare services are crucial to alleviate the burden on central hospitals and improve overall patient care efficiency [14]. Therefore, the implementation of studies such as this one is essential to inform policy and improve healthcare delivery.
Currently, few studies have been conducted to assess nurses' knowledge and skills in managing DFUs. To evaluate nurses' understanding of diabetic foot management, most studies have focused on specific areas of knowledge such as risk factors, foot examination, foot complications, and footwear selection [7-9, 15]. In this study, we developed a survey questionnaire specifically for Comprehensive Foot Examination and Risk Assessment. Through seven questions, the questionnaire explores nurses' knowledge related to the risks, symptoms, skin manifestations of DFU, the process of assessing vascular status, tests for assessing peripheral neuropathy in DFUs, and the preventive management of DFUs.
At the primary healthcare level in Vietnam, patients with DFUs are often hospitalized across various specialties, including the Trauma and Orthopedics, Cardiology, Endocrinology, and Neurology departments. Therefore, this study specifically focused on assessing nurses' knowledge of diabetic foot care within these departments.
Globally, nursing education on diabetic foot care varies significantly, with many countries lacking structured programs. In Vietnam, although nursing curricula include content on diabetes, there is limited emphasis on DFU management, which aligns with the trends reported in previous studies worldwide [13, 16]. Nurses' knowledge of DFU care is often acquired through self-study or participation in specialized scientific conferences. This has a substantial impact on the level of knowledge among nurses, as strongly demonstrated by the findings of this study. Nurses participating in this survey lacked comprehensive knowledge about DFU management. The number of questions that were answered by nurses reaching Level 1 gradually decreased. The majority of nurses (28.4%) answered only 1 question correctly at Level 1, while only two nurses (0.4%) answered all seven questions correctly. In contrast to Level 1, a higher percentage of nurses (24.3%) answered all seven questions at Level 2, and only 70 nurses (12.5%) answered one question at Level 2 (Table 2). The results of this study are consistent with the research of Yunita et al. (2022), who assessed the knowledge and attitudes of 396 nursing students toward diabetic ulcer care at three nursing schools in Indonesia from September 2021 to February 2022 [17]. The authors found that 43.2% (171/396) of the students had inadequate knowledge about diabetic ulcer care [17]. When examining nurses' knowledge of DFU, along with their practices and attitudes toward diabetic foot care, Mafusi et al. (2023) found that a significant proportion of nurses in Kimberley, South Africa, lacked adequate knowledge. The study emphasized the importance of continuous education and training programs to enhance nurses’ competency in DFU management [18]. While many nurses possess fundamental knowledge of DFU care, studies suggest that further education and training are necessary to deepen their understanding of peripheral neuropathy and related lower extremity complications [17]. In this study, nurses demonstrated gaps in knowledge regarding the following topics: “Risks of DFUs (Q1), Symptoms of neuropathy in the patient with DFUs (Q3), The foot cutaneous manifestations of DFUs (Q4), Tests that are commonly used to assess peripheral neuropathy in DFUs (Q6) and Preventive management (Q7)”. This is evident from the fact that a large proportion of nurses' responses to these questions were limited to Level 2. In contrast, topics in Question 2 (Medical history factors) and Question 5 (Procedures used to assess vascular status) are relatively straightforward and familiar in the daily clinical practice of nurses in Vietnam. Therefore, nurses' understanding of these two questions appeared somewhat better than others. However, the proportion of nurses who answered these questions (Q2 and Q5) at Level 1 was still relatively low, with only 45% and 54.8% of participants, respectively (Table 3). Overall, the findings of this study are generally consistent with previous research. Yunita S et al. (2022) found that among the 43.2% (171/396) of nursing students who had inadequate knowledge about DFUs, a higher proportion lacked an understanding of the characteristics of diabetic ulcers, diabetic neuropathy, and wound infection compared to other areas of knowledge [17].
4.2. Factors Associated with Nurses’ Knowledge
Understanding the factors influencing nurses' knowledge of DFU management is essential for enhancing the quality of patient care. Previous studies have explored a range of determinants, including gender, age, educational background, length of nursing experience, wound care experience, participation in wound care training, and hospital department [7-9, 15]. In the present study, three variables were selected for analysis: workplace setting, wound care experience, and participation in wound care training, as these were considered the most relevant characteristics of the study population.
The findings revealed that nurses who had received wound care training had significantly higher Level 1 knowledge and lower Level 2 knowledge compared to those who had not received training (Table 3). This result aligns with the study by Mafusi et al. (2024), which highlighted that inadequate or irregular training programs negatively impact nurses’ knowledge of diabetic foot management. The study emphasized that structured and continuous education is essential to enhance nurses' competencies in DFU care [18]. Similarly, Ramzan S et al. (2022) demonstrated that a 16-week diabetic foot care training program significantly improved both the knowledge and practice scores among nurses (p < 0.001), reinforcing the importance of structured education in this field [8]. Rasha et al. (2024) conducted a study to evaluate the effectiveness of a foot care training program for nurses caring for elderly diabetic patients. The study utilized a pre/post quasi-experimental design with 50 nurses and found that the training significantly improved both the nurses' knowledge and their foot care practices. Based on these findings, the authors recommended distributing the foot care booklet to nurses in other hospitals to enhance their knowledge and practices further [19].
Interestingly, this study found no significant association between workplace or wound care experience and nurses' knowledge of DFU management (Table 3). This contrasts with the findings of Kumarasinghe et al. (2018), who conducted a cross-sectional study across three teaching hospitals in Sri Lanka and found that nurses with extensive wound care experience and longer professional tenure achieved higher knowledge scores. The study also emphasized the importance of in-service education and peer knowledge sharing as crucial sources for updating nurses' knowledge. These findings highlight the significance of structured education and practical experience in improving clinical practices in DFU care [20]. Such discrepancies may be attributed to differences in study settings, sample characteristics, or methods of knowledge assessment, underscoring the need for further investigation.
Another possible explanation is that, in the Vietnamese healthcare setting, wound care experience may not necessarily involve exposure to evidence-based practices specific to DFU care. Additionally, the workplace environment may lack sufficient opportunities for continuing education or standardized protocols for DFU management, which could hinder knowledge acquisition despite practical experience [21]. Moreover, variations in the quality, frequency, and relevance of workplace training across departments may contribute to inconsistencies in knowledge acquisition. Some nurses may also have experience in treating non-specific or general wounds without direct exposure to the clinical management of DFU cases, thus limiting their domain-specific knowledge. These findings suggest that access to structured and formal training programs may be more influential in enhancing knowledge levels than clinical experience alone, as demonstrated in a study by Ramzan et al. (2022), which found that a targeted educational intervention significantly improved nurses’ knowledge and practices regarding DFU prevention in a tertiary care hospital setting [8]. Further research is warranted to explore the impact of diverse educational and clinical environments on nurses’ competencies in DFU care.
Overall, these findings underscore the critical importance of implementing structured wound care training programs to enhance nurses’ knowledge. They also highlight potential disparities in how workplace settings and clinical experience contribute to competency in DFU management. Future research should investigate strategies for optimizing training programs to ensure that both novice and experienced nurses receive comprehensive, evidence-based education, ultimately improving the quality of care for patients with DFUs.
Based on the study's findings, several strategies can be proposed to enhance the structure and effectiveness of DFU training programs for nurses. Firstly, training should be standardized and evidence-based, incorporating international guidelines such as those from the American Diabetes Association and the International Working Group on the Diabetic Foot (IWGDF) [22]. Structured modules should address key areas such as peripheral neuropathy, vascular assessment, foot care practices, and patient education to ensure comprehensive and current knowledge. Additionally, incorporating simulation-based education and case-based learning has been shown to significantly improve both theoretical understanding and clinical skills related to diabetic foot care, as demonstrated by Inkaya et al. (2020) [23]. Furthermore, integrating online education and blended learning models, as highlighted by Aminuddin et al. (2025) [24], has proven effective in enhancing knowledge and skills, particularly in resource-limited settings. These findings underscore the potential of e-learning platforms to improve clinical competencies in DFU prevention and management.
These strategies are well-positioned to address the knowledge gaps identified in this study, and contribute to the development of a highly competent nursing workforce capable of delivering effective DFU care.
4.3. Study Limitation
This study employed a descriptive cross-sectional design, which inherently limits the ability to establish causal relationships or assess changes over time. As such, longitudinal studies are recommended for future research to provide a more comprehensive and dynamic evaluation of nurses’ knowledge in DFU management.
Several methodological limitations may have influenced the findings. First, although the questionnaire included multiple-answer items, it lacked a confounding control scheme, potentially introducing bias in the interpretation of knowledge levels. Additionally, the absence of distractor options may have reduced response variability, and limited the ability to differentiate between partial and complete knowledge.
Measurement errors may also have occurred during data collection, including possible misunderstandings of the questions, variability in individual interpretations, and inconsistent answering behaviors among respondents. Furthermore, response bias is a concern, as participants may have either overestimated or underestimated their knowledge, particularly in items where self-perception or socially desirable responses could have influenced their answers.
To enhance validity and reliability in future research, more rigorous question validation procedures, including pilot testing and expert review, should be implemented. Additionally, mixed-method approaches, such as integrating qualitative interviews or observational assessments, could provide a more nuanced understanding of knowledge application in clinical practice and help address the limitations of self-administered surveys.
CONCLUSION
This study highlights substantial gaps in nurses’ knowledge of DFU management within primary healthcare settings in Northern Vietnam. Notably, neither workplace setting nor wound care experience was significantly associated with knowledge levels. In contrast, nurses who had received formal wound care training demonstrated significantly higher levels of knowledge.
These findings emphasize the critical need for structured and continuous DFU-specific training programs. Such programs should be integrated into both undergraduate nursing education and ongoing professional development initiatives. To maximize their impact, training content must be evidence-based, aligned with international guidelines, and tailored to the realities of primary healthcare in Vietnam. Addressing these educational gaps is essential for strengthening nurses’ competencies and improving patient outcomes in diabetic foot care.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: N.D., N.H.: Study conception and design; A.N., N.A.: Data collection; N.L.: Analysis and interpretation of results; P.D.: Draft manuscript. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| ADA | = American Diabetes Association |
| ABI | = Ankle-Brachial Index |
| DEPT | = Department |
| DFU | = Diabetic Foot Ulcers |
| ECBR | = Ethics Committee in Biomedical Research |
| Q | = Question |
| SpO2 | = Peripheral Capillary Oxygen Saturation. |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The research protocol was reviewed and approved by the Ethics Committee in Biomedical Research (ECBR) of the Vietnam National Burn Hospital, Vietnam (Approval No: 02/CNCHT-HDDD).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee, and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
All participants signed an informed consent form and provided consent for the publication.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the article's findings is available in the secured data repository of the National Burn Hospital at web [http://vienbongquocgia.vn], reference number [1578].
ACKNOWLEDGEMENTS
We would like to express our sincere gratitude to all our colleagues in the 12 northern provinces of Vietnam for their participation in the survey and for their enthusiastic support in this research.